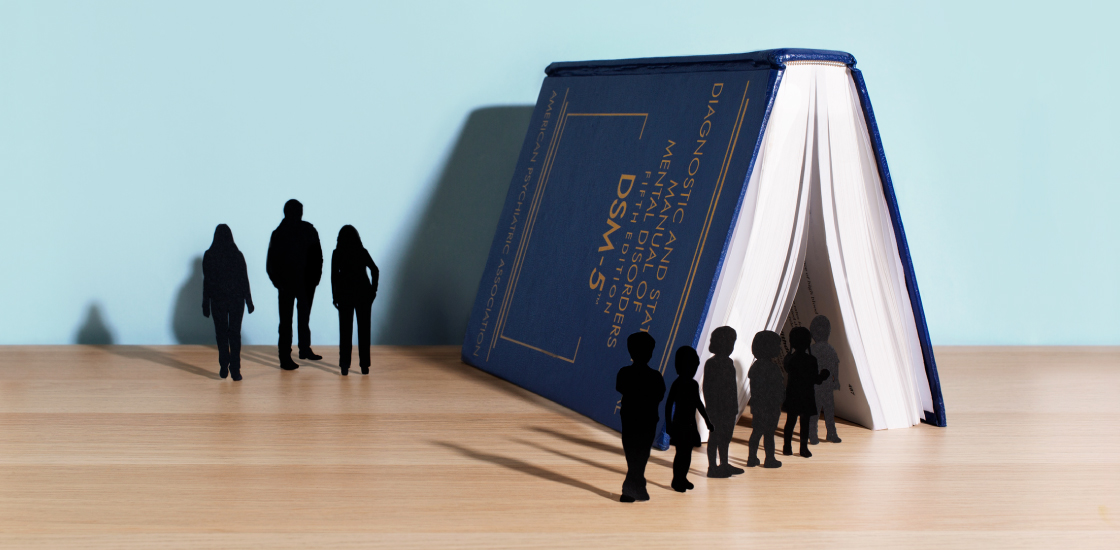
The DSM-5 has not improved services for autistic adults
Since the DSM-5’s debut, schoolchildren have gained stronger legal rights and better opportunities for accessing services; for adults, it’s a different story.
Editor’s Note
Spectrum’s house style is to refer to ‘people with autism’ rather than ‘autistic people.’ But we made an exception in this instance because of the author’s preference.
In early 2013, the then-emerging edition of the “Diagnostic and Statistical Manual of Mental Disorders” (DSM-5), proposed merging all autism diagnoses into a single category of ‘autism spectrum disorder.’
The Autistic Self Advocacy Network, the largest national organization run by and for autistic adults, strongly supported this move. In the view of the organization, where I now serve as executive director, the prior distinctions made no sense, did not reflect the experiences of autistic people and divided the efforts of advocates.
Critics of the unified definition feared that some people diagnosed with Asperger syndrome or pervasive developmental disorder-not otherwise specified (PDD-NOS) might not qualify for an autism diagnosis under the new criteria, and would be denied crucial assistance.
Five years on, that fear has proved unwarranted: Children have gained stronger legal rights and better opportunities for accessing services. ‘Autism’ is explicitly named in the Individuals with Disabilities Education Act, so having that diagnosis protects children from being denied services.
For adults, unfortunately, it’s a different story.
Services for autistic adults were always, and remain, woefully inadequate, leaving us without the supports we need to thrive.
The DSM-5 has done its part to unify us, but a manual cannot magically change laws, social barriers to diagnosis or misconceptions about what autism is.
The move toward diagnostic unity empowered self-advocates to join forces in the fight for civil and educational rights as well as adequate supports for autistic people. But getting services for autistic adults requires more than diagnostic tinkering. It requires lawmakers to address the hurdles that separate those with an autism diagnosis from the help they need.
Excluding autism:
One major obstacle is that the adult service system was designed to serve people with intellectual disabilities only. This requirement excludes most autistic adults.
It is tempting to assume that autistic people who speak fluently and have high intelligence quotients need less support than those who do not. But nothing could be further from the truth.
Autism is a developmental disability, and by definition, most of us need help on an ongoing basis. Some of us need that help only periodically, some need it every day, and some need it around the clock. Though the intensity of our needs varies, we will likely require roughly the same kinds of help, such as assistance with living in the community and with getting and keeping a job.
Home- and community-based services are desperately underfunded, causing pervasive problems with quality and a national shortage of support workers. More than 600,000 individuals with developmental disabilities, including many on the spectrum, are on waiting lists for these services in the United States. The waits usually last several years.
Eligibility for services such as transportation and employment assistance, as well as funding for housing, supersede the definitions in the DSM-5. Changing eligibility rules and new funding mechanisms would require new legislation, regardless of how autism is defined in the DSM.
Many people on the spectrum don’t even make it to a waiting list because they do not get a diagnosis in the first place. Women and girls, people of color, those from lower socioeconomic backgrounds, and those who do not speak English as a first language are all more likely to go undiagnosed or be to identified late in life in the U.S.
Here, too, the problem is not one that diagnostic criteria can fully solve, because it stems from diagnostic biases and societal and cultural barriers to medical care.
Stronger together:
A missed diagnosis in youth can mean no diagnosis at all, because doctors are really bad at spotting autism in adults. They often assume that if an adult were autistic, the person would have been diagnosed earlier. We also lack good assessments for adults.
Too many clinicians mistakenly believe that if you briefly make eye contact, say a sentence out loud or appear happy for a moment, you cannot be autistic. Indeed, the president of the San Francisco Bay Area Autism Society declared in January that if someone can mask any trait of autism for any period of time, that person cannot really be autistic.
These beliefs are false, but they may discourage people from seeking a diagnosis for themselves or a family member.
Advocates continue to make progress in dissolving service barriers and misconceptions about autism. Acting as one community has helped to drive that progress. Some people want to return to the pre-DSM5 subdivisions, but our community does not need more divisions.
The question isn’t: Should we have changed the diagnostic criteria? The question is: How do we connect the criteria in the DSM to the realities that confront us to make life better for autistic individuals?
Julia Bascom is executive director of the Autistic Self Advocacy Network.
Recommended reading
Explore more from The Transmitter

Neuro’s ark: How goats can model neurodegeneration