Drug that shifts brain’s signaling balance could treat autism
A drug that alters the balance of two key chemical messengers in the brain may help treat autism, suggests a proof-of-principle study.
A drug that alters the balance of two key chemical messengers in the brain may help treat autism, suggests a proof-of-principle study1.
In the study, researchers tested the effects of a drug called riluzole, which is approved as a treatment for amyotrophic lateral sclerosis, a neuromuscular disorder.
They found that in people with autism, the drug boosts brain levels of gamma-aminobutyric acid (GABA), which dampens brain signals, relative to levels of glutamate, which excites brain activity. This effect is opposite to that seen in the study’s controls.
The results support the theory that the balance between inhibitory and excitatory signals is altered in autism. The researchers say riluzole itself is not ideal for use in autism because of its broad effects. But their study suggests that a drug that restores this balance could treat the condition, even in adults.
“It’s very hopeful to think that the adult brain is responsive and can change,” says lead researcher Gráinne McAlonan, deputy head of forensic and neurodevelopmental science at King’s College London.
The findings, published 23 May in Translational Psychiatry, are intriguing but should be reproduced in a larger sample, says Stephen Moss, professor of neuroscience at Tufts University in Boston, who was not involved in the study. The study included 17 men with autism and 20 controls.
Balancing act:
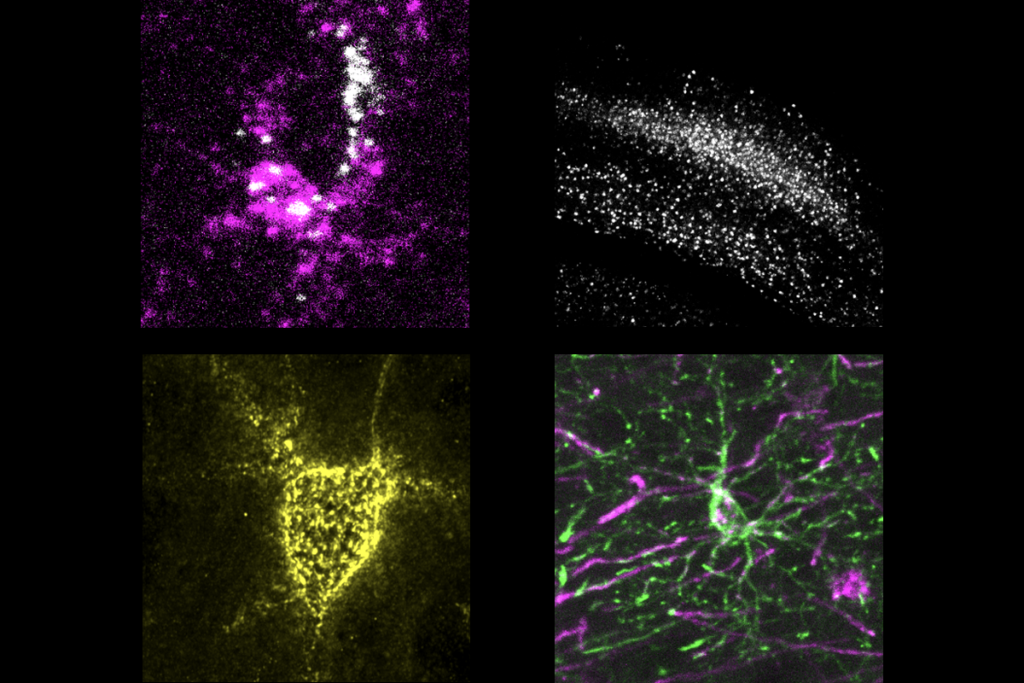
McAlonan and her colleagues used a technique called magnetic resonance spectroscopy, which detects magnetic signals generated by chemicals. They measured brain levels of GABA and glutamate.
Other studies using this technique in people with autism have yielded inconsistent results. But the studies measured the levels of a single chemical at one point in time, says McAlonan.
GABA and glutamate are in constant flux: GABA is synthesized from glutamate, which is made from glutamine. Glutamine can also be recycled from excess GABA and glutamate.
In the new study, the researchers measured GABA levels relative to the level of GABA, glutamate and glutamine combined. They did this twice in each participant: after giving them riluzole and after giving them a placebo.
They found that riluzole increased the proportion of GABA relative to the other chemicals in adults with autism and lowered it, albeit only slightly, in controls. The result suggests that people with autism regulate these chemicals differently than typical individuals do.
“When we try to think about drug development in the future, we can’t assume that the mechanisms that we see in a typical brain necessarily apply to someone with autism,” McAlonan says. “We need to understand the biology before we rush into clinical trials.”
Black box:
How riluzole might affect the brain is unclear; the drug has myriad effects on neurons, many of which are unknown.
“I would say [the researchers] provide good evidence that the balance is shifting. But how the drug is acting is always a black box — a super black box in this case,” Moss says.
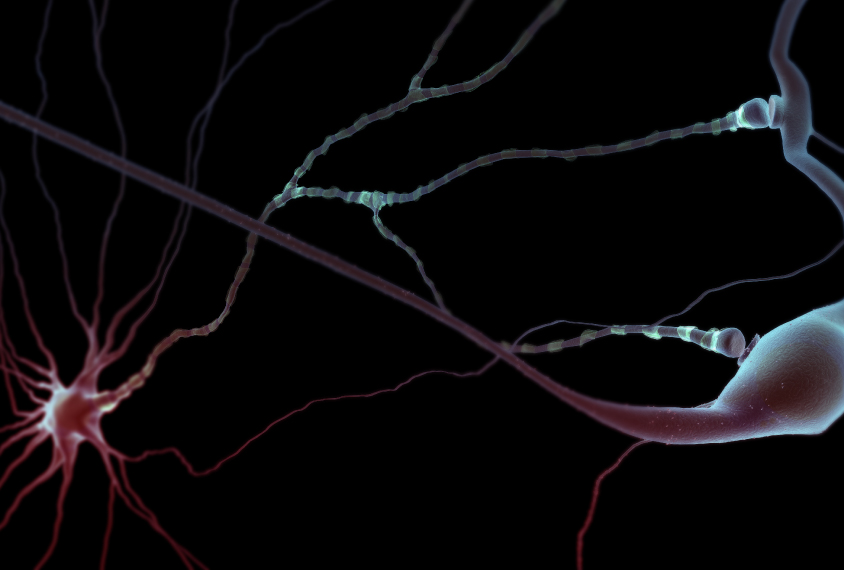
The researchers also used functional magnetic resonance imaging to analyze how well the brain’s center of planning and decision-making, the prefrontal cortex, communicates with the rest of the brain.
With placebo, the synchronization of activity between the prefrontal cortex and other brain regions was lower in people with autism than in controls. The drug normalized this synchrony in the participants with autism.
The researchers plan to repeat the study using other drugs that alter excitation and inhibition whose mechanisms are better understood, says McAlonan.
Although the researchers did not set out to test riluzole as a treatment for autism, other research teams are doing just that. Researchers presented preliminary results at the 2017 International Meeting for Autism Research in San Francisco showing that riluzole may alleviate hyperactivity and irritability in children with autism.
References:
- Ajram L.A. et al. Transl. Psychiatry 7, e1137 (2017) PubMed
Recommended reading
Explore more from The Transmitter