Drug improves gait in children with Phelan-McDermid syndrome
A new measure of motor skills suggests that insulin-like growth factor 1 improves movement in people with Phelan-McDermid syndrome.
A new measure of motor skills suggests that insulin-like growth factor 1 (IGF-1) improves movement in children with Phelan-McDermid syndrome. Researchers presented the unpublished findings yesterday at the 2017 Society for Neuroscience annual meeting in Washington, D.C.
IGF-1 is a hormone involved in fetal growth and is in trials to treat several autism-related conditions. It has been shown to improve social behavior and ease repetitive behaviors in children with Phelan-McDermid syndrome. The drug also reverses similar behaviors in mice.
Children with Phelan-McDermid syndrome often have trouble walking, pointing and rotating their joints. The new work is part of a clinical trial of an IGF-1 treatment for the condition.
“The first thing we did was measure their pre- and post-[treatment movements] and see if there was any overall change. And indeed, there was a huge change,” says Elizabeth Torres, associate professor of cognitive psychology and computational neuroscience at Rutgers University in New Jersey, who presented the work.
Torres’ team developed a model that involves using sensors to measure large and small movements. The sensors can measure micro movements, such as tiny rotations in an ankle joint, and detect changes even over a millisecond.
Gait gains:
Rather than predicting which improvements they might see, the researchers analyzed the data to spot differences in gait before and after treatment. They looked at movements in nine children with Phelan-McDermid syndrome. They assessed the movements before treatment, 12 weeks after treatment and at one follow-up visit.
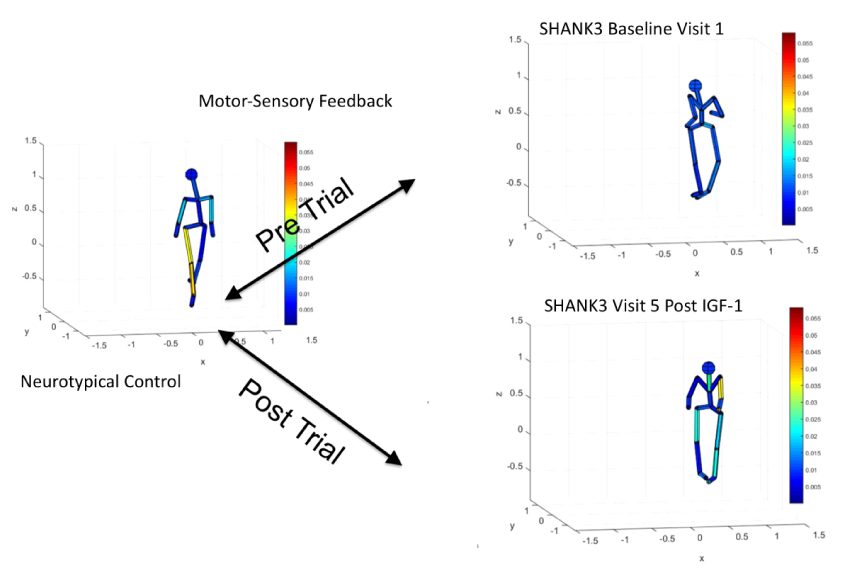
They then mapped the macro and micro movements captured by the sensors to create a map of movement in the feet, ankles and other body parts.
At baseline, the children with Phelan-McDermid had an irregular gait: They were unstable when they walked. And, unlike controls, they had no small, fast movements in their feet as they turned around.
After treatment, however, sensor maps of the children’s movements looked more similar to those of controls. For instance, the maps showed more fine-motor control in the children’s feet. The children also turned around more smoothly than before the treatment.
For more reports from the 2017 Society for Neuroscience annual meeting, please click here.
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter

This paper changed my life: Shane Liddelow on two papers that upended astrocyte research
Dean Buonomano explores the concept of time in neuroscience and physics

