Neurons are forever caught in a dance, adapting their signals to stay in step with new information. As the cells change pace, they need to maintain a delicate balance: If they ramp up excitatory signaling too much, it can lead to seizures; too much inhibition can lead to depressive or catatonic states.
Neurons strike this balance by way of processes collectively called homeostatic plasticity. Like a thermostat, this set of controls continuously dials excitatory and inhibitory signaling up or down as needed across our neural circuitry. Homeostatic plasticity explains how our brains stay plastic yet preserve their basic functions over time. It might also modulate autism traits, some experts say.
Over the past decade, research has shown that knocking out different autism-linked genes in various brain regions and cell types can disrupt homeostatic plasticity — findings that suggest it is a point of convergence for multiple forms of the condition. This work has also shown how homeostatic disruption leads to signaling imbalances that, according to one popular theory, give rise to some of autism’s characteristic traits, among them sensory hypersensitivity and motor difficulties.
Individual differences in homeostatic plasticity may even account for why autism traits vary so widely among people with the same genetic mutation, some scientists speculate.
“I don’t think there’s any direct data for it, but it would certainly be a very good hypothesis,” says Peter Kind, professor of developmental neuroscience at the University of Edinburgh. The factors that lead to variability in autism — including someone’s environment and genetic background — can also affect how brain circuits are regulated, Kind says. “So different mechanisms of homeostasis in different people could explain some of the variability and resilience differences in the expression of a given genetic mutation causing autism.”
However tantalizing, the connection between homeostatic plasticity and autism is far from certain. Researchers are grappling with scientific and methodological questions. And with the exception of some in vitro studies using human stem cells, much of the evidence comes from work in animal models, says Laura Andreae, senior lecturer in brain development and autism at King’s College London. How that translates to people remains to be seen.
“It’s a great time to work on this,” Andreae says. “It’s very much an emerging field.”
Stable dynamics:
Neurons reset the brain’s thermostat in multiple ways — and some of these mechanisms falter in mouse models of autism and related conditions, such as fragile X, Rett and Angelman syndromes, studies suggest.
If an eye patch deprives a control mouse’s visual cortex of input, for instance, neurons encoding information from the uncovered eye will typically increase their activity and their likelihood of firing to offset the loss on the other side.
Neither adjustment takes place in mice missing the autism-linked gene SHANK3, however, according to a 2020 study led by Gina Turrigiano, professor of vision sciences at Brandeis University in Waltham, Mass. Treating mice with the mood-stabilizing drug lithium restored both homeostatic processes in the mice, Turrigiano and her colleagues found. It also eased the animals’ repetitive behaviors.
But because SHANK3 is associated with other neurodevelopmental and psychiatric conditions, it’s impossible to say from the study’s results whether these homeostatic changes are specific to autism, she says. “My view is actually [that] SHANK3 is just an essential part of the synaptic machinery.”
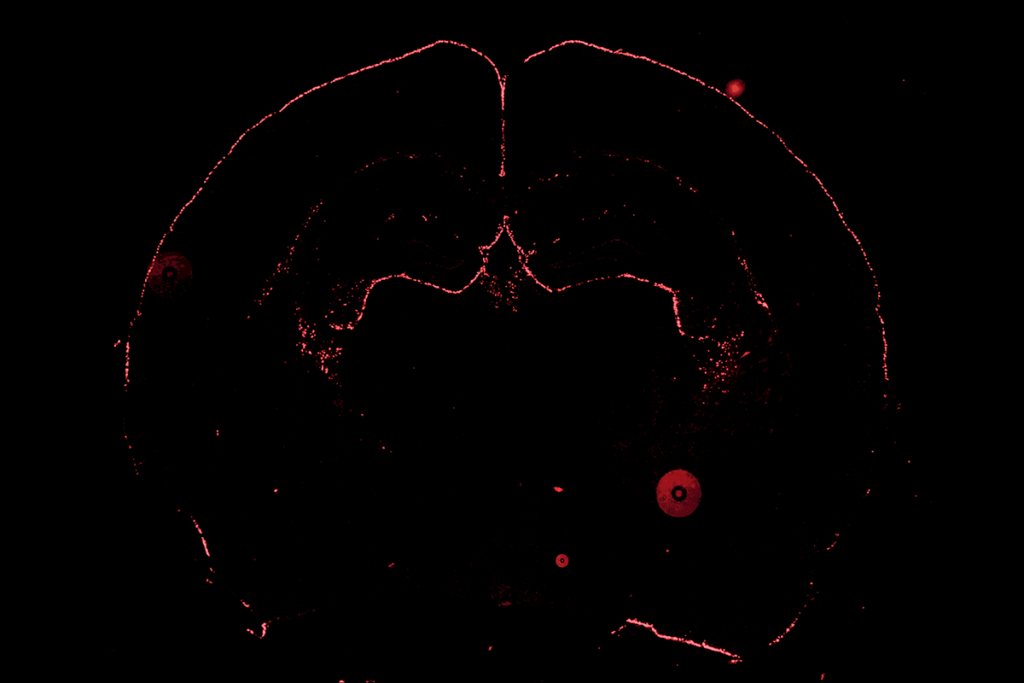
Mutations in another top autism-linked gene, CHD8, also appear to upset homeostatic plasticity in mice, according to an April study led by Andreae. Eliminating one copy of the gene in the animals’ prefrontal cortex — a brain region implicated in some of autism’s cognitive traits — led to a net increase in inhibition, the team found. The effect appeared to result from dampened and less frequent firing from excitatory cells and was most pronounced around 20 days after birth.
“There’s increasing evidence that these kinds of critical windows, if you have things that are changing, then that has knock-on effects for later behavior,” Andreae says.
Unsettled homeostatic processes may also drive Rett syndrome, other work reveals. The condition, characterized by repetitive behaviors and language delay, is almost always caused by mutations in MeCP2, which is involved in a homeostatic process called synaptic scaling: Blocking MeCP2 protein in mice prevents their synapses from adapting to signaling changes.
Brain slices from mice that model Angelman syndrome show signs of impaired synaptic plasticity. And in mouse models of fragile X syndrome, the animals’ neurons become overly excitable, a mark of homeostatic processes thrown off kilter.
“The immediate assumption is that [these homeostatic changes] have always been thought to be causally linked to downstream from the genetic mutation that you’re studying,” Kind says of his own work with fragile X mice. “But actually, whenever you find a phenotype, you never know.”
Compensation mechanisms:
The broader question — of whether autism-related mutations disrupt homeostatic plasticity directly, or those changes may be compensation — may be the biggest challenge the field faces, Kind says.
Distinguishing between the two will be key to devising therapeutics for people with autism, Kind says. Drugs designed to alter what may appear to be overly active or inactive brain regions could backfire if the activity is in fact a compensatory mechanism that serves to steady the brain.
Some compelling evidence suggests the changes are compensatory. For example, four mouse models all show an increase in the ratio of excitation to inhibition in neurons that process whisker movement, according to one 2019 study. But the mice do not show unusually high neuronal firing rates, as would be expected if the signaling shift were due to a direct hit to homeostatic plasticity. Instead, the neurons seem to boost overall excitation in ways that dampen and to some degree stabilize their firing rates.
“We concluded that, yeah, the [excitatory-inhibitory] ratio is changing in autism,” says Dan Feldman, professor of neurobiology at University of California, Berkeley, who led the work. “But it looks like it’s changing in a way that is successfully stabilizing synaptic function and perhaps the firing rate.”
To firm up the connection between autism and homeostatic plasticity, scientists will need to look at how genes affect several brain regions at once and identify what cell types drive neuronal changes, says Peter Wenner, professor of cell biology at Emory University in Atlanta.
“The focus in homeostatic plasticity has tended to be at the single-cell level,” he says. “But the cell by itself is not the critical feature. In my mind, it’s the network.”
Some of this work has already begun: Researchers are employing tools that use multiple electrodes to monitor activity in multiple areas of the brain in freely moving animals, Wenner says. In this way, they might collect data to weigh how different cell types, layers and brain regions respond to disruptions in homeostatic plasticity.
Advances may also come from comparative studies involving several mouse models to find common genes affecting homeostatic plasticity, Feldman adds. “Autism is such a diverse condition. You really need multiple models if you’re going to have an understanding about how a mechanism contributes to autism in general.”
Ultimately, as researchers learn more about the mechanisms involved with various mutations, they may be able to parse autism into smaller categories, with some more or less related to homeostatic plasticity, Andreae says. But for now, with myriad genes involved and limited tools to uncover how they interact to produce traits, it’s still difficult to get a holistic understanding of how homeostatic plasticity may be impaired in autistic people.
“It’s hard to find a consensus,” Andreae says, “because everyone’s kind of still trying to work out what’s going on.”