Complex gene interactions in autism offer avenues for treatment
Teasing out how genes interact can offer clues to autism’s causes and point to treatment targets.
Every scientific hypothesis comes with a set of assumptions. For example, we assume that a gene will play the same role in mice that it does in people, or that children will behave similarly in a research study as in the real world.
A common assumption in genetic studies is that each gene acts independently of all others. But we know that genes don’t act independently; they interact with one another. The effects of these interactions, called ‘epistasis,’ make it difficult to predict the impact of genetic variants tied to a particular condition, such as autism. But they also present new opportunities to understand a condition’s causes, potential biomarkers and treatment targets.
For instance, we know that high blood serotonin levels, which are associated with autism, run in families. In a 2004 study, my colleagues and I looked for genes that influence these levels1. We found an association between blood serotonin levels and the gene ITGB3. The gene doesn’t play an obvious role in regulating serotonin levels, but it is known to be expressed at the cell membrane, as is the serotonin transporter gene, SLC6A4. We hypothesized that the two genes may interact, and we showed that they genetically interact to contribute to autism risk2. Other groups later verified this finding3,4,5.
Researchers have since shown in mice that ITGB3 and SLC6A4 interact in the brain to regulate serotonin uptake6. Clinical studies of antidepressant drugs, many of which target the serotonin system, revealed that increased expression of ITGB3 is associated with better drug response among individuals with depression7.
Identifying a gene-gene interaction clarified how ITGB3 influences serotonin levels and autism risk. It also revealed a biomarker for an individual’s response to antidepressants. It’s possible this was a lucky break, but I believe the same approach can offer more clues about autism.
Uncovering interactions:
Studies in model organisms, such as mice, fruit flies, worms and yeast, suggest epistasis determines the majority of variation among individuals for complex traits, including behavioral traits. In fact, the contribution of genes working in combination to yield traits in mice and fruit flies appears to dwarf the contribution of genes acting alone8,9,10,11. But it is still unclear whether the same is true for people12.
Research using electronic medical records that include diagnoses of single-gene disorders such as fragile X syndrome, as well as those of complex conditions such as autism, strongly suggests that epistasis contributes to many medically relevant complex traits, including autism13. But few studies have comprehensively examined the contribution of epistasis to common human conditions.
One reason for the lack of such studies is the number of people required to find a signal. It takes DNA from tens of thousands of people with a particular condition to link common genetic variants in a single gene to that condition. Now consider all the variation in the genome in all of the two-way combinations — the odds are stacked against us.
We know that our ability to detect any genetic signal depends on the frequency of a given variant and how large an effect it has. And we know that the more common a variant is, the smaller effect it is likely to have.
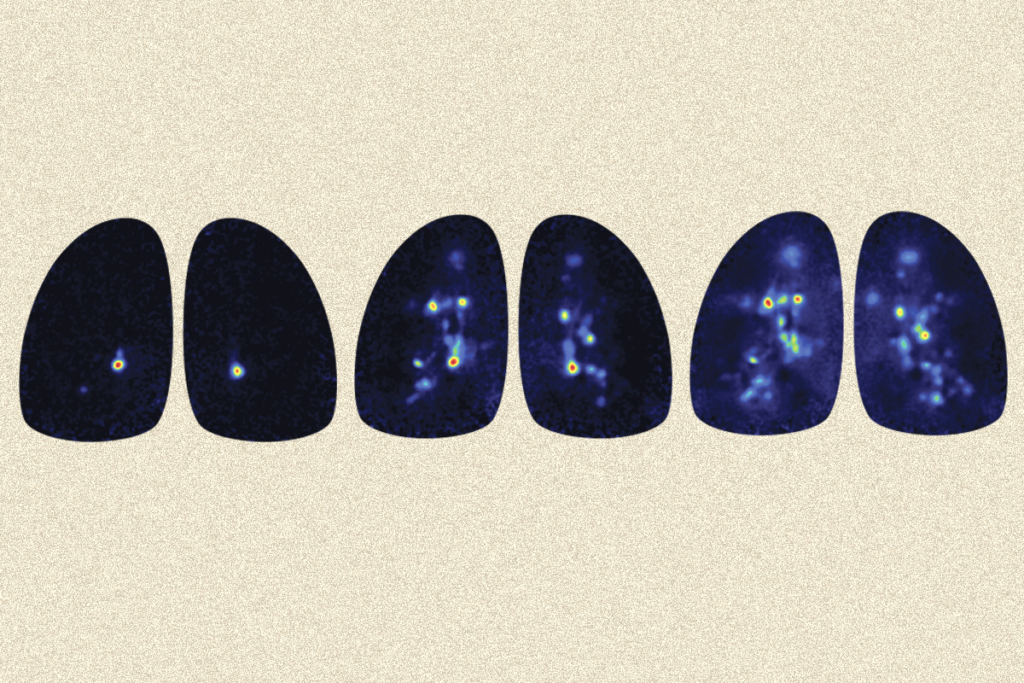
We decided to use the relationship between effect size and frequency to our advantage by using information from rare disorders to help identify common risk factors involved in autism. We used information from disorders called RASopathies, which are linked to autism and arise from a known glitch in a single molecular pathway, called Ras/MAPK.
First clues:
We tested our hypothesis by first looking for common variants that determine which people with one of these rare genetic conditions develop autism features. We were limited by the number of study participants (257) with RASopathies, so the results did not reach statistical significance, but we found some promising candidates14.
We also took a second approach, based on the assumption that the same biological pathways are likely to act in single-gene forms of autism as well as more common forms of the condition. This allowed us to narrow our search for epistasis in idiopathic autism (autism of unknown cause) by proposing that one in the pair of interacting genes would be in a specific biological pathway — the Ras/MAPK pathway.
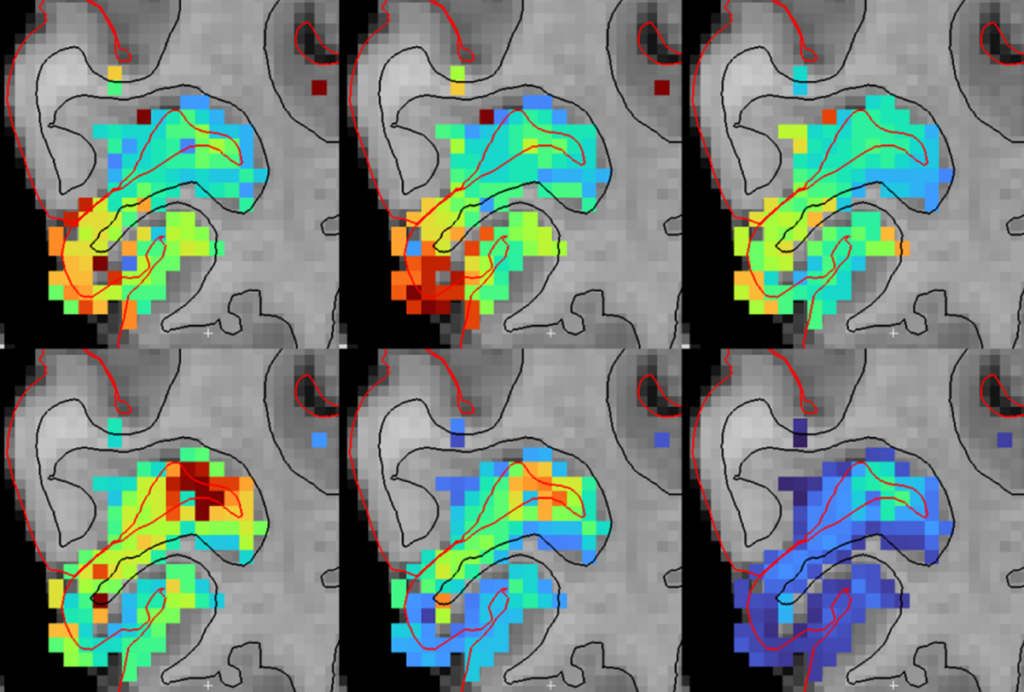
We took this second approach in a group of more than 4,000 ‘trios,’ which include people with idiopathic autism and their unaffected parents. In this group, we identified 19 independent, statistically significant pairs of interacting genetic regions14.
Many of the genes near the interacting variants make biological sense, either because they intersect with the Ras/MAPK pathway relevant to RASopathies or because they have been implicated in autism already.
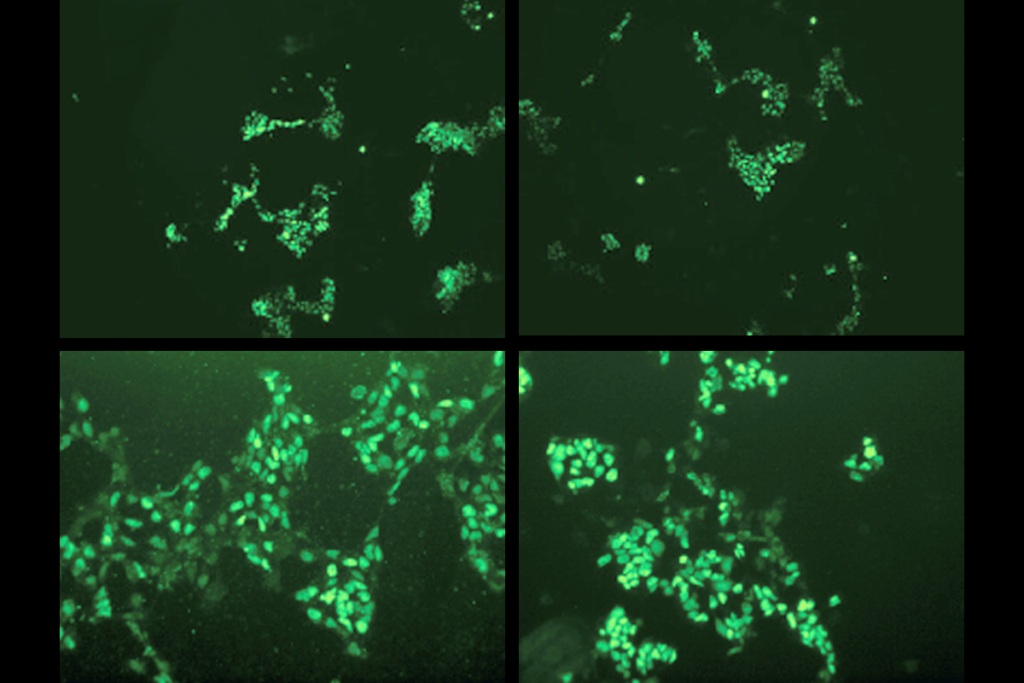
One of the top regions to emerge from this approach also turned up as a key region of interest in our study of people with RASopathies. This region contains a gene no one has studied yet, called GPR141. We found that expression of the gene is decreased in neurons derived the from skin cells of a person with a RASopathy. This condition, called cardio-facio-cutaneous syndrome, is associated with autism15.
We hope to learn much from these new results. We plan to study the functions of the specific pairs of genes implicated. We can apply a similar approach to other pathways or other conditions. And we can be creative about how to use ‘big-data’ resources, such as electronic health records, to detect epistasis. The time has come to face the complexity of genetic risk factors for autism head on.
Lauren Weiss is associate professor of psychiatry at the University of California, San Francisco.
References:
- Weiss L.A. et al. Eur. J. Hum. Genet. 12, 949-954 (2004) PubMed
- Weiss L.A. et al. Hum. Genet. 120, 93-100 (2006) PubMed
- Ma D.Q. et al. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 153B, 477-483 (2010) PubMed
- Coutinho A.M. et al. Hum. Genet. 121, 243-256 (2007) PubMed
- Mei H. et al. Am. J. Hum. Genet. 81, 1251-1261 (2007) PubMed
- Whyte A. et al. Neurochem. Int. 73, 122-126 (2014) PubMed
- Probst-Schendzielorz K. et al. Pharmacogenomics 16, 689-701 (2015) PubMed
- Shao H. et al. Proc. Natl. Acad. Sci. USA 105, 19910-19914 (2008) PubMed
- Gale G.D. et al. Mol. Psychiatry 14, 631-645 (2009) PubMed
- Huang W. et al. Proc. Natl. Acad. Sci. USA 109, 15553-15559 (2012) PubMed
- Bloom J.S. et al. Nature 494, 234-237 (2013) PubMed
- Hill W.G. et al. PLOS Genet. 4, e1000008 (2008) PubMed
- Blair D.R. et al. Cell 155, 70-80 (2013) PubMed
- Mitra I. et al. PLOS Genet. 13, e1006516 (2017) PubMed
- Adviento B. et al. J. Med. Genet. 51, 10-20 (2014) PubMed
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter
Smell studies often use unnaturally high odor concentrations, analysis reveals
‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt