Clinics unroll genome tests for undiagnosed disorders
Two university-based clinics have debuted large programs that rely on sequencing to diagnose genetic disorders, including developmental disorders such as autism.
Over the past few years, teams of scientists have been finding genetic glitches related to a wide variety of disorders by sequencing exomes, the protein-coding portions of the genome. But these genetic tests are typically out of reach for people unless they enroll in research studies, and even then, they’re almost never privy to their individual results.
But that looks set to change: A few clinics are debuting large programs that rely on sequencing of exomes or even of whole genomes, and making the results directly available to individuals. For less than $10,000 each, the tests offer people with unexplained genetic disorders the chance to find the cause of their condition.
The first academic lab to offer clinical exome sequencing was the Whole Genome Laboratory at Baylor College of Medicine in Houston. Since November 2011, the lab has sequenced the exomes of some 1,700 individuals with undiagnosed conditions, including many children with developmental disorders. It now averages about 200 exomes a month.
“It’s gone gangbusters,” says Richard Gibbs, director of Baylor’s Human Genome Sequencing Center, which helped establish the new lab. The researchers have pinpointed the genetic cause of about one-quarter of the 1,700 cases as mutations in known disease genes, he says.
Last week, the Harvard-affiliated Partners Healthcare Center in Boston launched a similar lab focused on sequencing whole genomes. And two private companies — Ambry Genetics in Aliso Viejo, California, and GeneDx in Gaithersburg, Maryland — have offered clinical exome sequencing since 2011.
Deciding which parts of the sequencing data should be divulged to individuals is far from straightforward. A few mutations are clearly associated with disease, but most are still tricky to interpret.
From a research perspective, however, the development is unequivocally exciting, experts say.
That’s because at clinics affiliated with academic institutions, participants may choose to contribute their de-identified data into freely available databases that researchers can tap for their studies. That could prove a huge advantage for researchers funded by agencies such as the National Institutes of Health (NIH).
“A ton more samples can be screened in the clinic than can be screened in NIH-funded studies,” says Jonathan Sebat, associate professor of psychiatry at the University of California, San Diego. “That’s ultimately what’s going to drive discovery forward.”
Sharing genomes:
Many clinical tests already exist for undiagnosed developmental disorders. These tests typically screen a single gene or a panel of genes for certain rare variants, which appear only in a few people, or common variants, which crop up in at least five percent of the general population.
Whole-exome and whole-genome sequencing, in contrast, read the genome one nucleotide at a time. Because of their scale and expense, these used to be rarely used techniques, but as costs have plummeted, scientists have greatly accelerated the pace of sequencing. Researchers are learning not only how to interpret the troves of data, but how to securely store and manage it.
Baylor, for example, has sequenced about 20,000 exomes — mostly from healthy people or from tumors of people with cancer — for research studies.
“We were doing so many of these exomes in the research setting, and developing expertise around interpretation and solving genetic disease,” Gibbs says. “We wanted to transfer that capability over to a clinical environment.”
Clinical laboratories must meet regulatory standards that don’t exist for research labs. Notably, the federal Clinical Laboratory Improvement Amendments program mandates that all clinical labs must follow a strict set of operating and quality control procedures.
Baylor’s new lab charges $7,500 for a child’s exome sequence, according to Gibbs. In most cases, it then screens small portions of the parents’ genomes to determine whether certain mutations are spontaneous — that is, not inherited from the parents — and potentially causative.
The Partners group plans to offer clinical whole-genome sequencing for $9,000 each, according to Heidi Rehm, director of Partners’ Laboratory for Molecular Medicine, which will run the tests. The researchers have sequenced a handful of genomes so far and have found the genetic underpinnings of two cases, both adults, Rehm says.
But many of the cases are likely to be of children with undiagnosed developmental disorders.
“Exome and genome testing really allows you to explore many different potential causes for those disorders in a broad approach,” Rehm says. Still, “this doesn’t mean that overnight we’re going to solve all of these cases.”
The Partners and Baylor labs both intend to ask participating families to consider contributing their data for research purposes.
There is precedent for clinical genetic data being used for research purposes. For years, academic clinical labs and private companies have collected data on copy number variations — deletions or duplications of DNA — in children with undiagnosed developmental disorders. A significant portion of that information has gone into publicly available repositories, such as the International Standards for Cytogenomic Arrays Consortium.
“We created a database and evidence-based review process so we could help labs determine what was clearly pathogenic and clearly benign,” says David Ledbetter, one of the founders of that repository and chief scientific officer of Geisinger Health System in Danville, Pennsylvania. Last year, Ledbetter’s group combined data from two such databases to find several new variants associated with autism.
“Now we need to do the same thing for exome sequencing,” he says.
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

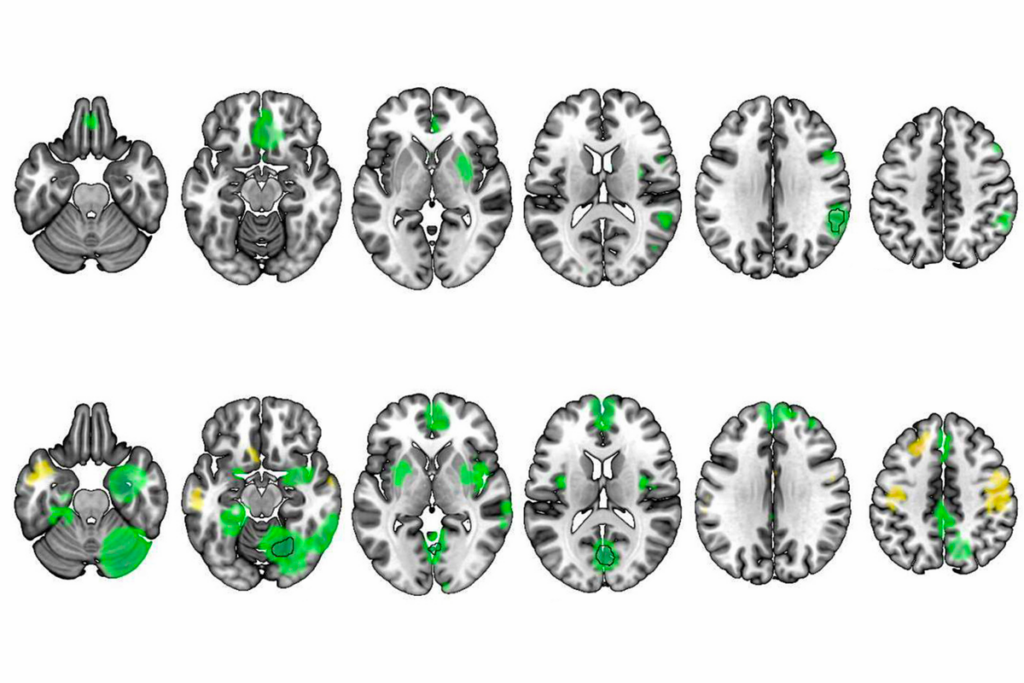
Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter
Emotional dysregulation; NMDA receptor variation; frank autism
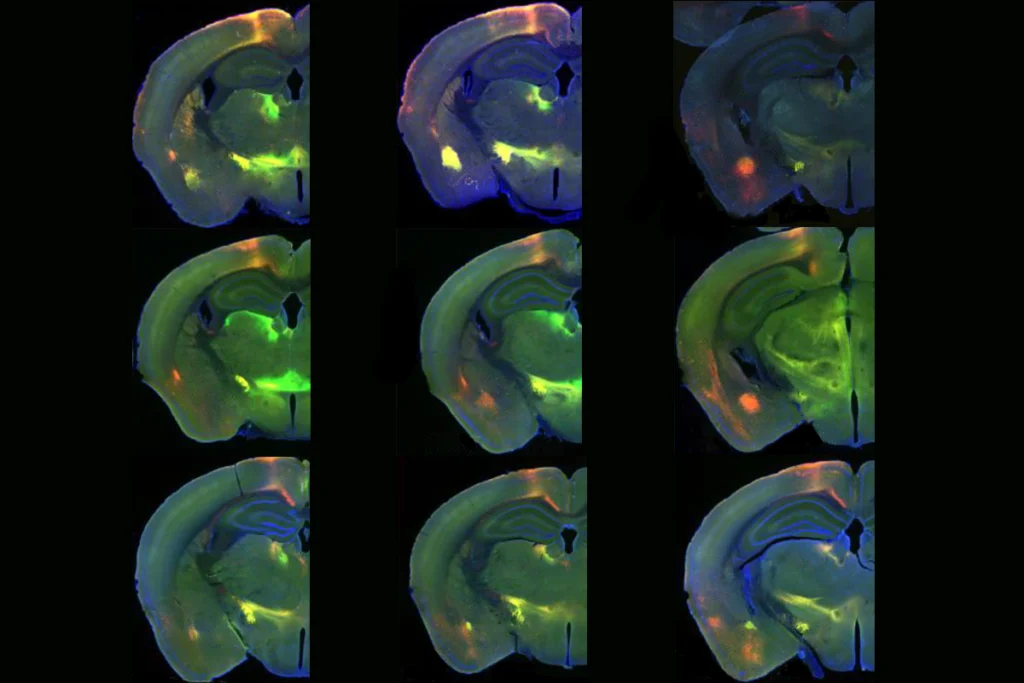
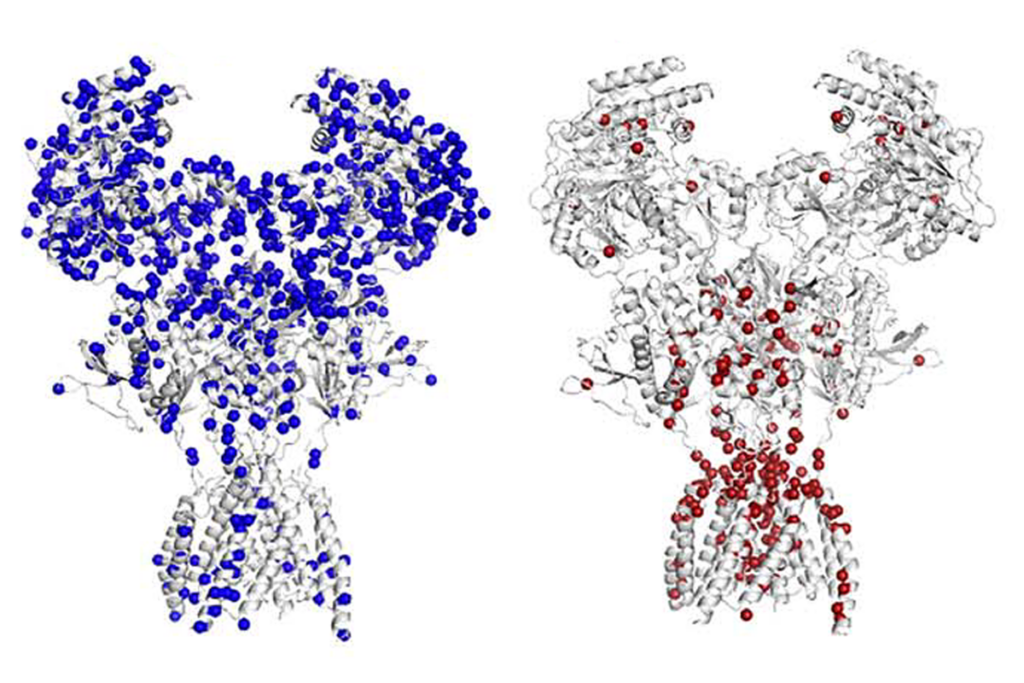
Newfound gene network controls long-range connections between emotional, cognitive brain areas