Welcome to this month’s edition of the By the Numbers Newsletter. At Spectrum, we do our best to summarize the latest autism research findings — and sometimes the best summary comes in the form of a chart or map. In this newsletter, we boil down interesting new research that is conveyed most succinctly by way of data visualizations.
Let us know what you think of the newsletter, or tell us about your own data-rich work, at [email protected].
Machine learning and neuroimaging
Machine-learning models may be better at spotting signs of autism in brain scans if the datasets include women, according to a new analysis of data from 44 studies.
“We want to improve the data that is used for machine learning because, you know, ‘garbage in, garbage out,’” says lead investigator Sotirios Bisdas, a neuroradiologist at the National Hospital for Neurology in London, England. The goal of the new study, Bisdas says, was “to understand whether there are systemic biases that affect the data quality and, downstream, may affect results.”
The answer, it turned out, is yes: Some types of neuroimaging data, such as electroencephalography, are potentially better than others for training machine-learning models to identify autism, the study shows. Including women and data from multiple imaging technologies may also improve the sensitivity and specificity of some machine-learning algorithms.
Machine learning is unlikely to aid autism diagnosis any time soon. There is wide variability in how autism shows up in boys and girls, how the condition is diagnosed, how neuroimaging is performed, and in the machine-learning algorithms used to draw conclusions from data.
To improve the accuracy of machine learning algorithms, Bisdas says, researchers should first standardize imaging methods.
“It doesn’t make sense to wait for more imaging data if we don’t standardize its collection,” Bisdas says. “Yes, we need more data, but we need more quality data.”
The results appeared in Neuroradiology in August.
Early-onset dementia and autism
About 4 percent of adults with autism were diagnosed with early-onset dementia between 2008 and 2012, compared with less than 1 percent of non-autistic adults, according to a new study. The prevalence is more than 5 percent amongst people with both autism and intellectual disability.
The data came from Medicaid Analytic eXtract and included more than 1.2 million adults who received Medicaid benefits between the ages of 30 and 64. More than 12,000 people in the dataset have autism, 511 of whom were diagnosed with dementia before the age of 65. Among those with autism, the prevalence of early-onset dementia was higher for Black than for white people; it was also higher for those living in rural areas compared with city-dwellers.
The findings appeared in Autism Research in August.
Spectrum story spotlight: Prenatal exposure to antipsychotics does not increase autism odds
Children born to women who take antipsychotic medications during pregnancy, such as aripiprazole or risperidone, do not have elevated odds of having autism or attention deficit hyperactivity disorder, nor are they more likely to be born preterm or underweight, according to a study published in JAMA Internal Medicine in August.
Prescribing antipsychotics during pregnancy can help prevent potentially dangerous psychotic episodes and ensure that an expectant mother can take care of herself, says Mady Hornig, associate professor of epidemiology at Columbia University, who was not involved in the study. “We certainly don’t want to be cavalier about the use of any medication during pregnancy, but one also wants to balance out the implications of not treating.”
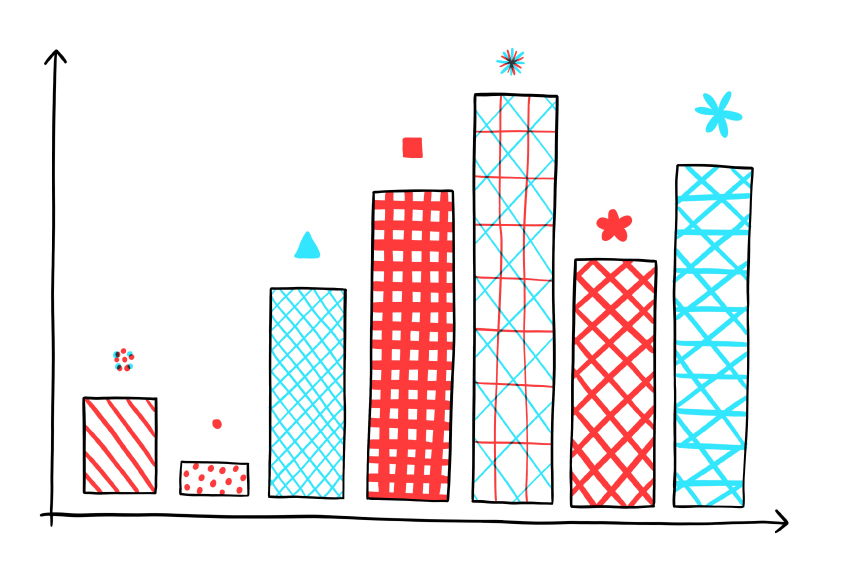
Any apparent effects of antipsychotics on a developing fetus are likely due to the condition that is being treated, rather than the treatment itself, the study shows. That’s because doctors prescribe medications for a specific reason, which can lead to additional differences between women who do and don’t take medications, and can skew study results. This explains why women who were medicated during pregnancy appear to have an increased hazard ratio for giving birth to children with autism, as shown in the chart above.
The findings appeared in JAMA Internal Medicine in August.
Spectrum index:
27: The number of co-occurring conditions, such as epilepsy and intellectual disability, that affect significantly more women than men with autism. The results appeared in the Journal of the American Medical Informatics Association in August.
336.6 percent: The increase in autistic adults who received supplementary security income awards, a U.S. cash assistance program, in 2019 compared with 2005. The greatest increases were in New Jersey, Delaware and Connecticut, according to a study published in the Journal of Autism and Developmental Disorders in August.
1.35: The increased odds that an autistic person’s cousin will have depression, compared with someone not related to an autistic person. The result, published in the Journal of Child Psychology and Psychiatry in August, drew on data from nearly 2.4 million people in Sweden. Many other conditions, including anxiety, eating and psychotic disorders, were also more common among relatives of people diagnosed with autism.
Dataset spotlight: A new longitudinal dataset of the developing mouse brain, created using resting-state functional connectivity data on the cortex, tracks postnatal development from a batch of animals across time. A preprint describing the data appeared on bioRxiv in April.