Brain tissue study bolsters autism, schizophrenia link
Brains from people with autism show patterns of gene expression similar to those from people with schizophrenia.
Brains from people with autism show patterns of gene expression similar to those from people with schizophrenia, according to a new analysis1.
The findings, published 24 May in Translational Psychiatry, deepen the connections between the two conditions, says study leader Dan Arking, associate professor of genetic medicine at Johns Hopkins University in Baltimore, Maryland.
People who have either autism or schizophrenia share features such as language problems and difficulty understanding other people’s thoughts and feelings. They also have genetic risk factors in common. “And now I think we can show that they share overlap in gene expression,” Arking says.
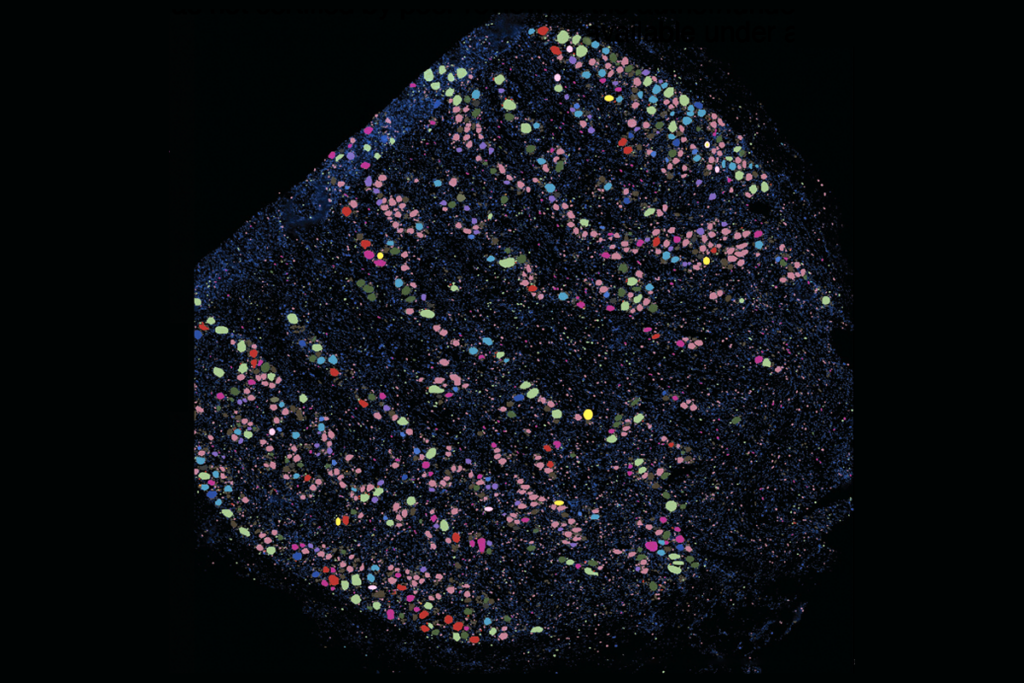
The study builds on previous work, in which Arking’s team characterized gene expression in postmortem brain tissue from 32 individuals with autism and 40 controls2. In the new analysis, the researchers made use of that dataset as well as one from the Stanley Medical Research Institute that looked at 31 people with schizophrenia, 25 with bipolar disorder and 26 controls3.
They found 106 genes expressed at lower levels in autism and schizophrenia brains than in controls. These genes are involved in the development of neurons, especially the formation of the long projections that carry nerve signals and the development of the junctions, or synapses, between one cell and the next. The results are consistent with those from previous studies indicating a role for genes involved in brain development in both conditions.
“On the one hand, it’s exciting because it tells us that there’s a lot of overlap,” says Jeremy Willsey, assistant professor of psychiatry at the University of California, San Francisco, who was not involved in the work. “On the other hand, these are fairly general things that are overlapping.”
Strong ties:
Most previous studies of gene expression in autism or schizophrenia did not involve brain tissue: Some relied on blood and others on neurons derived from stem cells. “Having what the brain transcriptome looks like is important,” says Jon McClellan, professor of psychiatry at the University of Washington in Seattle, who was not involved in the work.
It’s also significant that the common patterns emerged from two disparate datasets involving different study designs and brain regions. “The fact that you have a positive finding, to me, under those circumstances, really says that this is likely to be real,” Arking says.
In the study, gene expression in schizophrenia and bipolar disorder are not notably similar, even though schizophrenia is thought to have stronger genetic ties to bipolar disorder than to autism. A larger study may reveal an overlap between the two conditions, Arking and others say.
The similarities in gene expression between schizophrenia and autism could stem from a shared mechanism for the two conditions. Or they may reflect common processes that compensate for the other brain changes, says Shannon Ellis, who conducted the analysis as a graduate student in Arking’s lab. “We can’t say anything about whether this is cause or effect,” she says.
Flagging genes:
By comparing the results of genetic studies with gene expression analyses, researchers can glean hints about causal relationships. The genes that show altered expression in people with autism or schizophrenia are not ones that tend to pop up in genome-wide association studies of these disorders. Those studies are designed to reveal common variants that occur more often in people with a condition than in the general population.
The disparate results from these different kinds of studies suggests that the gene expression changes in autism and schizophrenia brains don’t cause the conditions, Arking says. “What we’re seeing are sort of the downstream consequences of that primary effect,” he says.
The study does point to new genes that may play a role in the conditions. Two genes located on chromosome 12, called IQSEC3 and COPS7A, are expressed at unusually low levels in autism, schizophrenia and bipolar disorder, the researchers found.
Relatively little is known about these two genes, and they may not be involved in all cases of these conditions. Still, they are worth following up on, says Arking. IQSEC3, in particular, is dramatically suppressed in all three conditions. “It’s hard to imagine that’s not an important player in some way,” he says.
References:
Syndication
This article was republished in Scientific American.
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures

Glutamate receptors, mRNA transcripts and SYNGAP1; and more
Explore more from The Transmitter
‘Unprecedented’ dorsal root ganglion atlas captures 22 types of human sensory neurons

Not playing around: Why neuroscience needs toy models

