Autism is a neurodevelopmental condition. Although it is diagnosed based on the presence of two core behaviors — restricted interests and repetitive behaviors, as well as difficulties with social interactions and communication — those traits are thought to arise because of alterations in how different parts of the brain form and connect to one another.
No research has uncovered a ‘characteristic’ brain structure for autism, meaning that no single pattern of changes appears in every autistic person. Studies of brain structure often turn up dissimilar results — there is great variety across individuals in general. But some trends have begun to emerge for subsets of autistic people. These differences might one day provide some insight into how some autistic people’s brains function. They may also point to bespoke treatments for particular subtypes of autism.
Here is what we know about how brain structure differs between people with and without autism.
Which brain regions are known to be structurally different between autistic and non-autistic people?
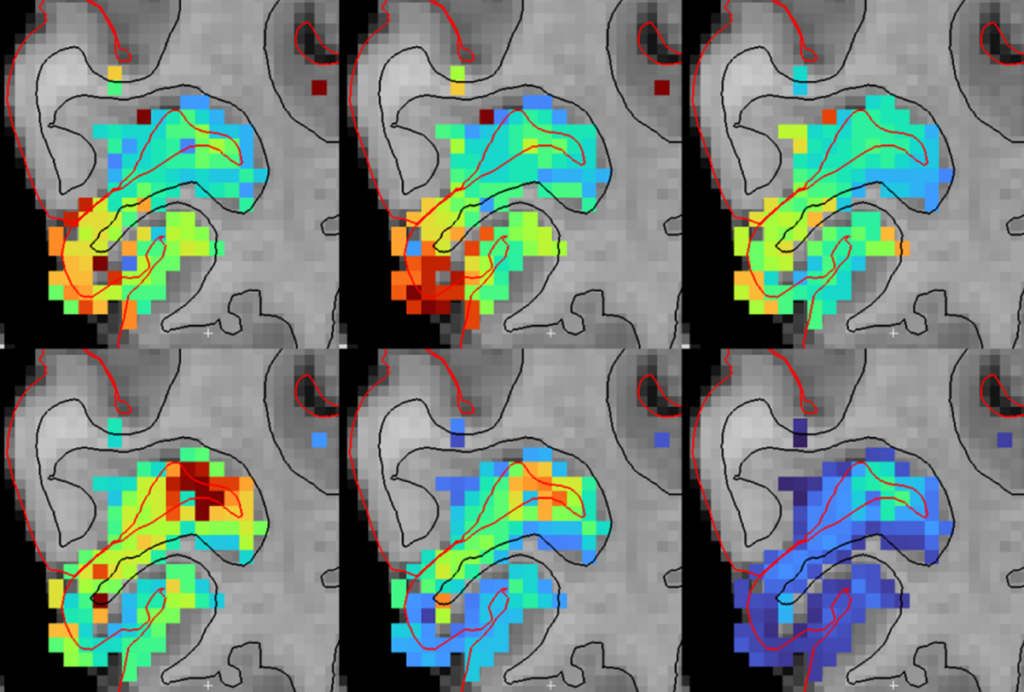
Studies that make use of a brain-scanning technique called magnetic resonance imaging (MRI) have highlighted a few brain regions that are structurally distinct in people with autism.
Children and adolescents with autism often have an enlarged hippocampus, the area of the brain responsible for forming and storing memories, several studies suggest, but it is unclear if that difference persists into adolescence and adulthood1,2.
The size of the amygdala also seems to differ between people with and without autism, although researchers from different labs have turned up conflicting results. Some find that people with autism have smaller amygdalae than people without autism, or that their amygdalae are only smaller if they also have anxiety3. Others have found that autistic children have enlarged amygdalae early in development and that the difference levels off over time2,4.
Autistic people have decreased amounts of brain tissue in parts of the cerebellum, the brain structure at the base of the skull, according to a meta-analysis of 17 imaging studies5. Scientists long thought the cerebellum mostly coordinates movements, but they now understand it plays a role in cognition and social interaction as well.
On a more global level, the cortex — the brain’s outer layer — seems to have a different pattern of thickness in people with and without autism. This difference tracks with alterations to a single type of neuron during development, a 2020 study suggests.
How do these structural differences change during development?
Some infants who are later diagnosed with autism have unusually fast growth in certain brain regions, according to multiple studies6,7,8. Compared with their non-autistic peers, autistic children have significantly faster expansion of the surface area of their cortex from 6 to 12 months of age. In the second year of life, brain volume increases much faster in autistic children than in their non-autistic peers.
The results support earlier research that saw enlarged heads and brains in a fraction of autistic people: Their cortex seems to expand too quickly in infancy and early childhood, even before autism traits can be detected behaviorally. During late childhood, neurotypical brains continue to grow in size; in adulthood, they begin to shrink. By contrast, the brains of some people with autism start to shrink prematurely, before their mid-20s.
Some children who are later diagnosed with autism also have excess cerebrospinal fluid — the liquid that surrounds the brain — compared with their non-autistic peers, which may contribute to having an enlarged head. Those with the most fluid tend to also have the most prominent autism traits later in life7. The excess fluid appears as early as 6 months of age and persists through age 39.
What about the structure of the connections between brain regions?
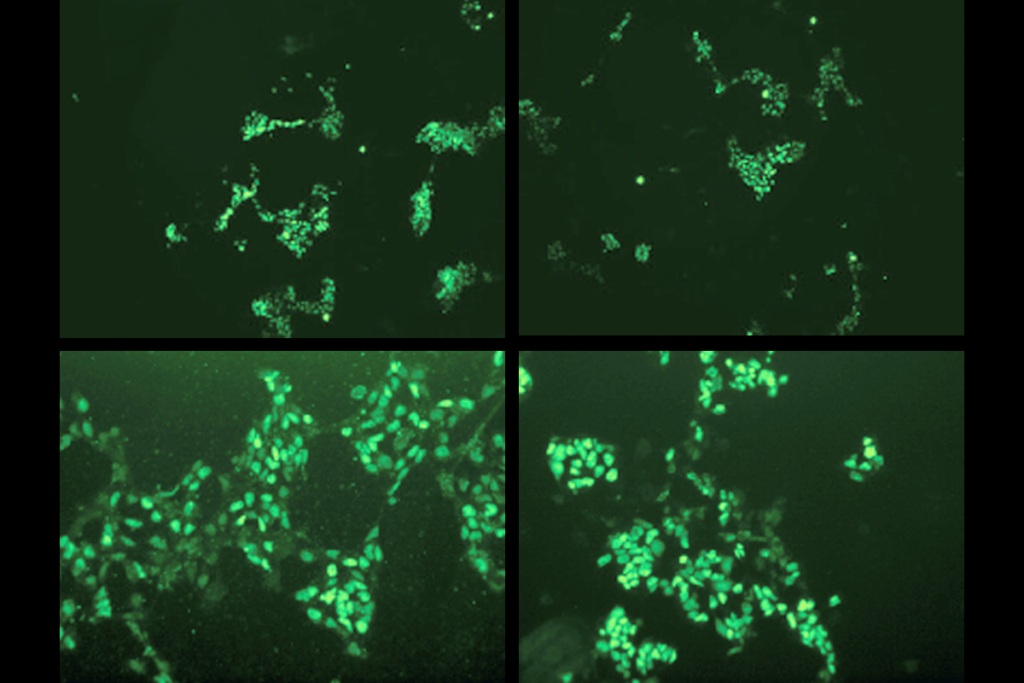
A solid body of evidence suggests that white matter, the bundles of long neuron fibers that connect brain regions, is also altered in people with autism. Researchers typically infer the structure of white matter by using a technique called diffusion MRI, which measures the flow of water throughout the brain.
People who lack all or part of one white matter tract called the corpus callosum, which connects the brain’s two hemispheres, have an increased likelihood of being autistic or having traits of the condition10. The corpus callosum contains many of the long-range connections that extend throughout the brain; the fact that disrupting those connections may lead to autism traits supports the connectivity theory of autism.
Preschoolers with autism show significant differences in the structure of multiple white-matter tracts, according to a 2020 study. Autistic toddlers and adolescents, too, show alterations in white matter throughout the brain11,12.
Are there sex differences in the brain structure of people with autism?
It’s unclear. Identifying sex differences in autism remains challenging because fewer girls than boys are diagnosed with autism, says Mark Shen, assistant professor of psychiatry at the University of North Carolina at Chapel Hill.
Still, a few recent studies have turned up hints of sex differences in the brain in autism. A 2020 study showed that the amygdala is more affected in autistic girls than in autistic boys13. An enlarged amygdala is associated with more severe emotional problems specifically in autistic girls, according to other work.
White-matter changes in preschoolers with autism also differ by sex: Autistic girls have an increased measure of structural integrity in their corpus callosum compared with non-autistic girls, whereas that measure is lower in autistic boys than in non-autistic boys14.
Other structural differences, such as the rate of brain growth and amount of cerebrospinal fluid, appear similar between the sexes6,9.
Why is brain structure in autism important to study?
Because autism is a heterogeneous condition, “when we talk about autism, we’re probably talking about different biological subtypes,” Shen says.
Though not every baby who is later diagnosed with autism will have excess brain fluid at 6 months of age, and not every autistic adult has an underdeveloped corpus callosum, learning more about these subtypes can help researchers develop biologically based treatments for individuals with autism.
Additionally, finding structural biomarkers that can identify subtypes of autism in a noninvasive way, even before autism behaviors can be detected, will help “move the needle earlier” for autism diagnoses, Shen says.