Certain rare autism-linked mutations alter brain structure in distinct ways, according to a new study. But they affect other aspects of a person’s health in similar ways, influencing the cardiovascular system in particular.
Copy number variants (CNVs) — deletions or duplications of large stretches of DNA — have long been linked to neurodevelopmental and psychiatric conditions. The mutations likely have effects beyond the brain, but their rarity has made those effects difficult to identify, says study investigator Jakub Kopal, a postdoctoral researcher in Danilo Bzdok’s lab at McGill University in Montreal, Canada.
“These mutations are in every cell of your body,” Kopal says.
Kopal and his colleagues developed a new approach to circumvent the inherently small sample sizes. They identified structural brain imaging patterns associated with each of eight mutations and found additional people who have those same patterns in the UK Biobank, a database of brain, medical and socioeconomic data from half a million residents of the United Kingdom. They then uncovered the traits tied to those brain patterns.
Though people with different CNVs have distinct brain signatures, they have similar physical phenotypes, the researchers found. That convergence reinforces the theory that the molecular underpinnings of many brain-related conditions overlap, says Andres Moreno De Luca, assistant professor of autism and developmental medicine at Geisinger in Lewisburg, Pennsylvania, who was not involved in the work.
“It was a pretty sophisticated and elegant study,” Moreno De Luca says. “This paper adds more data to prove the point that there is no such thing as an ‘autism only’ gene.”
The approach could be used to study any condition or disease in large datasets such as the UK Biobank or the ABCD study, Kopal says.
“You don’t necessarily need patients with the diagnosis to be able to study the disease,” he says. “You just need a thing that clearly separates your group of patients from healthy controls.”
T
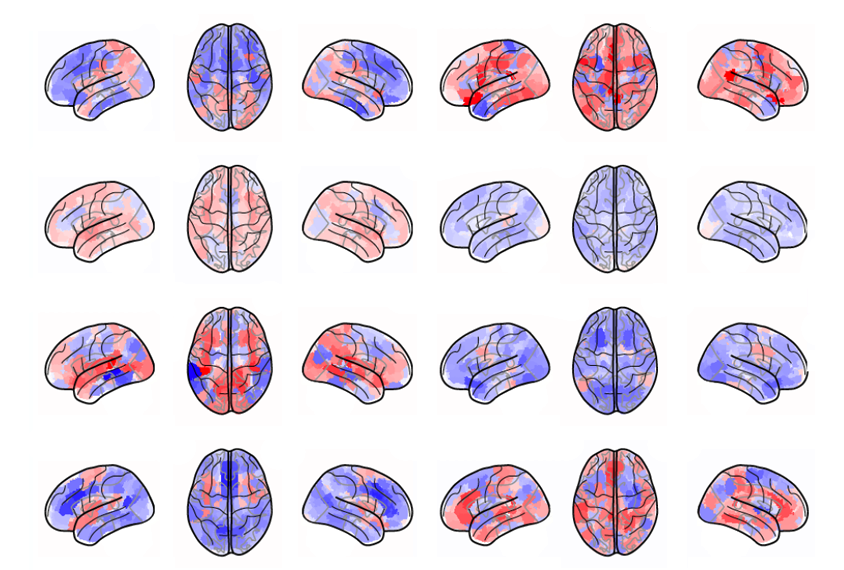
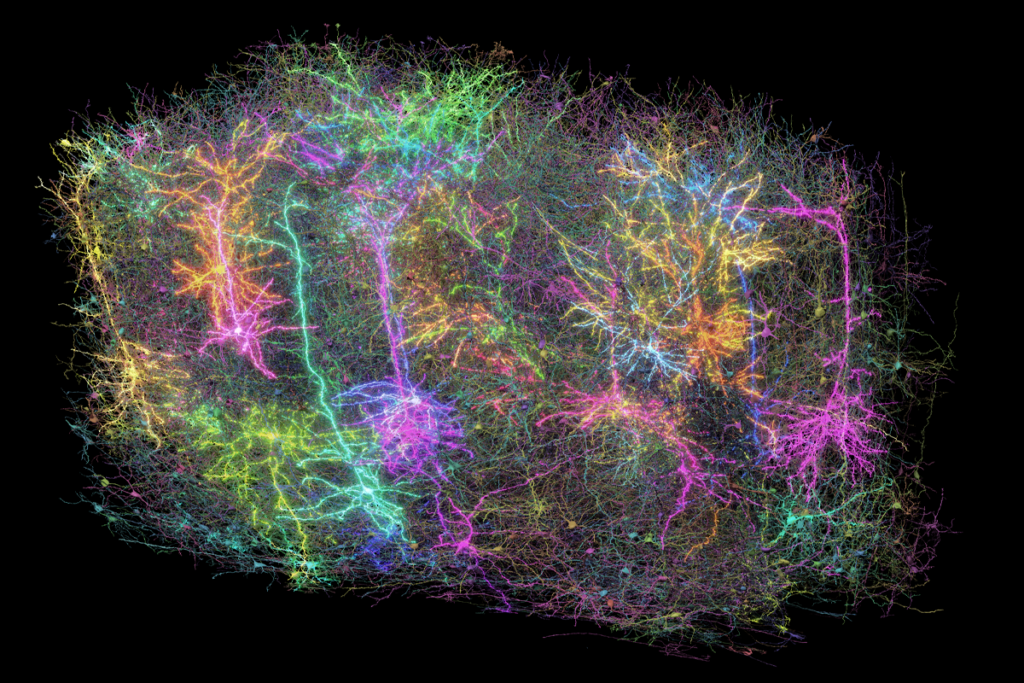
he researchers analyzed MRI data from 534 people with a deletion or duplication in one of four genetic loci — 1q21.1, 15q11.2, 16p11.2 or 22q11.2 — and 312 controls. People with 1q21.1 deletion, 15q11.2 duplication, 16p11.2 duplication and 22q11.2 deletion showed reductions in brain volume, whereas those with the remaining mutations showed increases. Deletions and duplications in the same loci tended to show opposite effects.The limbic network, which is involved in behavioral and emotional responses, was the most frequently affected area across the eight mutations, the researchers found. The 16p11.2 deletion affected the largest number of brain regions, and the 15q11.2 duplication affected the fewest.
The imaging patterns accurately predicted a person’s CNV, suggesting they could serve as a signature of someone’s condition, Kopal says.
He and his colleagues then generated a score for each of 39,085 people from the UK Biobank that indicated how closely their brains matched each mutational signature and looked for associations between those scores and 977 biological and sociodemographic attributes.
People with brains similar to those with any of the CNVs tended to share similar diastolic blood pressure readings, red blood cell counts and cholesterol levels, among other traits. They also shared some lifestyle factors, such as the amount of alcohol they drink.
The findings were published in Nature Human Behavior on 2 March.
T
he work suggests that researchers studying neuropsychiatric conditions need to examine factors outside of the brain, particular those associated with the heart, says Sundari Chetty, assistant professor of psychiatry at Harvard Medical School, who was not involved in the work.“It’s very, very interesting and novel,” she says. “This now brings to attention that we need to look at the interactions between cardiovascular factors and how it impacts the brain.”
It will be important to see if the findings also apply to autistic people without a known genetic condition, she says.
The brain architecture of autistic people with 22q11.2 deletion is distinct from that of autistic people without the deletion, according to a 2020 study from an independent team.
Clinicians who see children with these mutations should be aware that cardiac issues are likely to emerge later in life, Kopal says.
The technique could also help researchers better understand how common and rare variants interact, Moreno De Luca says.
“It would be nice to have a model where you flow that in as well, which is where I think the field is going,” he says. “Having that in mind for the next version of this — that would be great.”