Bits of bacteria may change brains of fetal mice
Bacterial fragments can cross the placenta of a pregnant mouse into the brains of her developing pups, leading to a surplus of neurons in the pups.
Bacterial fragments can cross the placenta of a pregnant mouse into the brains of her developing pups, leading to a surplus of neurons in the pups, along with learning deficits later on, suggests a new study.
The results jibe with others indicating that some people with autism have an excess of neurons in certain regions of the brain.
“The architecture of what the brain should look like is fundamentally different [in these mice], and that, I think, is really totally surprising,” says lead investigator Elaine Tuomanen, chair of infectious diseases at St. Jude Children’s Research Hospital in Memphis, Tennessee. The work appeared 9 March in Cell Host & Microbe1.
Infection during pregnancy can raise the risk of autism in the child by about 37 percent, according to one epidemiological study. Although researchers are still teasing out the biological basis of this link, work in mice and rats suggests that a mother’s immune system produces molecules that can affect the fetal brain.
The new study hints at a different mechanism. “You might not need the maternal inflammation to produce the effects observed [in the brain], but rather a piece of the bacteria itself can trigger the process in the fetus,” says Harley Kornblum, professor of psychiatry, pharmacology and pediatrics at the University of California, Los Angeles, who was not involved in the study.
Exactly how the bacterial pieces increase neuron numbers in the fetal brain is unclear. The net rise in neurons could stem at least partly from a decline in the number of cells dying rather than from an increase in cell division, some experts say. The study also did not show that the brain changes in the fetal mice persist into adulthood.
Still, the idea that a pathogen could directly change the developing brain represents a promising avenue for exploration, says Judy Van de Water, professor of internal medicine at the University of California, Davis, who was not involved in the study. “It’s a nice addition to the concept of how immune activation during gestation can change the course of neurodevelopment,” she says.
Moving pieces:
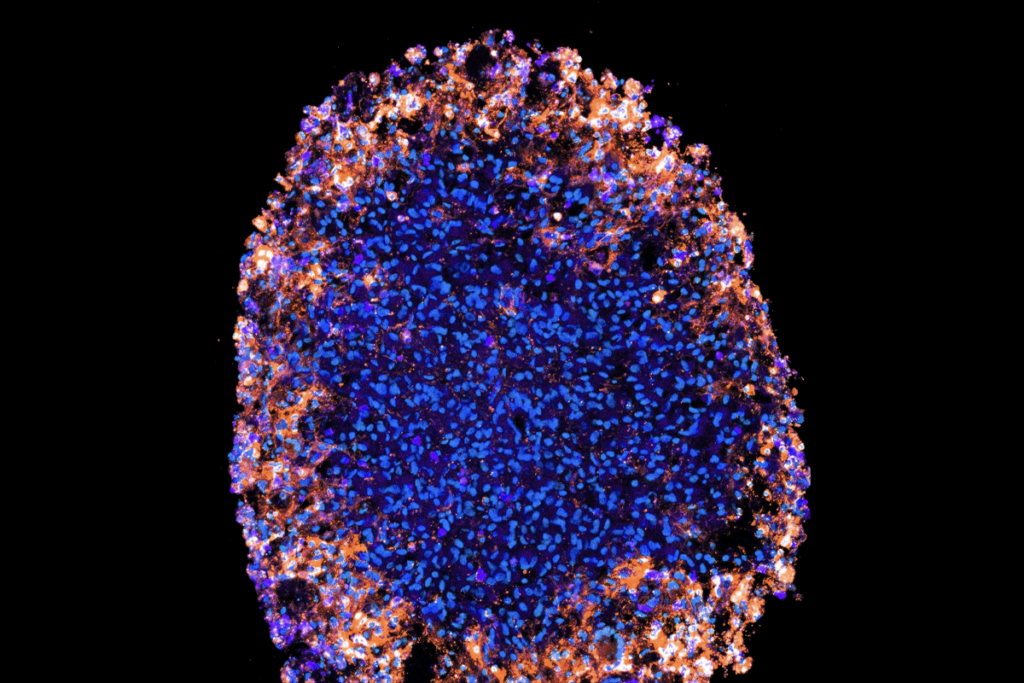
Tuomanen and her colleagues isolated the outer shell, or cell wall, of Streptococcus pneumoniae, which causes respiratory infections in people, and injected it into the bloodstream of pregnant mice. Within 24 hours, the bacterial molecules accumulated in the placenta and fetal cortex — the developing brain’s outer layer.
Six days later, the researchers saw a 50 percent increase in the number of neurons in the fetal cortex relative to the brains of unexposed pups. The rise in cell number coincides with an increase in expression of FOXG1, a gene that helps orchestrate fetal brain development and has been implicated in autism. Intriguingly, when the same microbial morsels are injected into an adult mouse, they cause a decrease in neuron numbers and an increase in the levels of markers for neuron death.
When the pups were 3 months old, they spent less time than controls sniffing an unfamiliar object. At 5 months, they spent less time exploring areas of a multi-chamber cage that had previously been blocked off. These findings suggest that the mice have problems with learning and memory, the researchers say.
To confirm that the bacterial pieces need to cross the placenta to exert their effects on the brain, the researchers injected pregnant mice with a modified cell wall that cannot pass from the blood into surrounding tissues. They saw no change in the number of dividing neurons or in FOXG1 expression in the pups’ brains.
Similarly, pups lacking a protein that transports bacterial cell wall from the bloodstream into tissue, or an immune protein that recognizes and binds to the bacterial fragments, show no brain changes. These findings suggest that the proteins are essential for the increase in neuron numbers.
Millions of pieces:
Although the researchers saw molecular markers of cell division in the fetal brain, they did not conclusively show that the cells divide faster or more frequently in the presence of the bacterial fragments, says Flora Vaccarino, professor of neuroscience at Yale University, who was not involved in the study. Nor did the researchers rule out diminished rates of cell death as a cause of the net increase in the number of neurons, she says.
It is also unclear which cell-wall molecules are responsible for the effects, says Ivo Gomperts Boneca, head of research on the biology and genetics of the bacterial cell wall at the Institut Pasteur in Paris. He says it is possible that bacterial molecules other than those in the cell wall are the real triggers for the brain changes. “What they’re seeing probably is true, but I’m not sure it is mediated, as they’re claiming, by the cell wall itself,” Boneca says.
Tuomanen and her colleagues also injected pregnant mice with live bacteria and treated them with an antibiotic that causes those microbes to break apart. Her team reported a surplus of neurons in fetal pups from these mice, too. If the finding holds up in people, it could raise concerns about the use of similar types of antibiotics during pregnancy.
“We know that the bacteria literally explode when you use those antibiotics, and so you create, from one bacteria, millions of pieces,” Tuomanen says. “You have to use something because you don’t want the person to die of infection, but potentially the antibiotics we’re using may not be the best choice.”
Tuomanen and her colleagues are sifting through existing epidemiological data for a link between antibiotic use during pregnancy and neurological conditions in children. Finding a connection would be an important first step toward altering clinical practice, she says.
References:
- Humann J. et al. Cell Host Microbe 19, 388-399 (2016) PubMed
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter
Dispute erupts over universal cortical brain-wave claim
Waves of calcium activity dictate eye structure in flies