Banking on brains for clues to autism
New initiatives aim to increase brain donations for autism research and maximize what scientists can learn from these precious specimens.
L
eslie Bolen was there for every one of her son Michael’s medical tests. He’d had more than his fair share in his 14 years, but this last one was almost too much for his mother to bear.That test was on a Saturday night in April 2016. Eight days earlier, Michael had had a seizure at the residential facility where he lived. He had autism, and he’d had seizures almost every week since he was 8 years old, but never one this bad. He stopped breathing, and his heart stopped beating. Medics managed to restart his heart with a shot of adrenaline, but his brain never recovered.
Michael spent the following week on life support. His parents rarely left his side, ducking out of the hospital only three times for clean clothes and to spend time with their then-13-year-old daughter, Rachel. Sitting in a chair beside Michael’s bed, Bolen played back events from the previous Friday in her mind: the frantic call from Michael’s caseworker, the seemingly endless 10-minute drive to the hospital, the look on her husband Chad’s face when he arrived at the hospital.
As part of the final test, doctors pinched Michael’s chest and poured ice water in his ear. Michael showed no response to these normally painful stimuli, confirming that he would never regain consciousness. For some of that time, his mother had prayed in the next room; heartbroken and exhausted, she focused on practicalities: She and her husband had already decided that they would donate his organs, because Rachel had benefited from a corneal transplant as an infant. But what about Michael’s brain?
Bolen Googled ‘autism brain donation’ on her phone and dialed the number on the screen. About 16 hours later, she joined the ranks of more than 350 families that have donated a loved one’s brain to autism research. “Michael died for a reason. I have to believe that, otherwise I can’t go on; maybe this was [the reason],” she says.
These decisions, however painful for families, are invaluable to researchers. Much of autism research has relied on mice, whose behaviors and brains are a far cry from those of people. Studying postmortem brains has revealed the pathological hallmarks of many neurological conditions — including Alzheimer’s disease, Parkinson’s disease and multiple sclerosis. Postmortem autism studies present unique challenges, however. Autism is much more heterogeneous than most neurological conditions. Researchers don’t yet know of any obvious features that distinguish the brains of people with autism. Whatever is present is likely to be subtle, and to vary from brain to brain. “You can be sure that every case is different,” says Patrick Hof, director of the Seaver Autism Center Tissue Program at the Icahn School of Medicine at Mount Sinai in New York City. “If you want to look for neuropathology and find patterns of cell pathology in these brains, you’re going to need numbers.”
Finding brains for autism research has another, thornier, complication. Whereas most people with Alzheimer’s or Parkinson’s diseases die in their 70s or 80s, autism is a developmental condition: The brains of children are most pertinent to research, but those who die usually do so unexpectedly, after drowning or having a seizure, for example. Getting enough numbers to definitively tie any feature to autism means reaching out to families in their darkest hour. A brain that sits unpreserved after death rapidly decays: After 24 hours, genetic messages inside the tissue start to fade; after 36 hours, the walls of each cell start to crumble. Depending on where the family is, and their proximity to a medical examiner and a tissue bank, there might not be a minute to spare.

Given all of these difficulties, there have been few brains available for autism research. In 1998, the advocacy group Autism Speaks launched the Autism Tissue Program — an effort to collect and distribute brain tissue for autism research. In 2013, the National Institutes of Health launched its own brain bank, the NIH NeuroBioBank, to collect brains for studying a wide range of conditions, including autism. But the two efforts had different protocols for processing and distributing samples. Neither had a wide reach across the United States, which meant some families were unable to donate even if they wanted to. “A lot of times, we would get brain authorization and not have a research home for it,” says Jason Bridge, vice president of eye and tissue services for Unyts, an organ procurement organization based in Buffalo, New York.
New initiatives in the U.S. and Europe aim to boost the number of autism brains by streamlining the donation process. They try to engage families long before death occurs, and they are working with hospitals, organ procurement organizations and medical examiners around the country to reach families immediately after the loss of a loved one. “People have to know us and be convinced that this is a good thing to do,” Hof says.
Protective measures:
T
he call for autism brains grew particularly urgent five years ago. In May 2012, a freezer at Harvard University containing about 50 specimens from the Autism Tissue Program — roughly one-third of the collection — malfunctioned. The freezer had two separate alarm systems, neither of which activated when the temperature began to climb above -80 degrees Celsius. The contents slowly thawed, destroying the cells in the tissues and degrading their scientific value. Scientists realized they needed better procedures to protect and distribute this limited resource.“My first thought really was, ‘Oh my gosh, this is a tragedy,’” says Eric Courchesne, professor of neuroscience at the University of California, San Diego. “You can always collect new DNA samples, you can always collect new RNA, you can always do new brain scans,” he says. But a physical brain? “It’s irreplaceable.”
The living brain is guarded by three layers of mesh-like tissue called meninges, the hard bones of the skull and a thin cushion of fluid in between that helps absorb shocks. But these protections were no match for Michael’s self-injurious urges. He once smashed his head against the windshield of his school bus so hard that the glass fractured into a spiderweb of cracks.
Michael was diagnosed with autism at 21 months. Bolen, who has an older son from a previous relationship, knew something was off when Michael swapped babbling and pointing for spinning and ‘stimming’ — self-stimulating behaviors. He loved to watch liquids seep into the carpet or couch, and so he would sometimes empty jugs of milk or orange juice or urinate right in the living room. Within a year of his diagnosis, he began hurting himself, at first slapping his head and then banging it against the wall or the floor.

Michael’s self-injury worsened as he grew. When he was 6, a neurologist ordered brain scans, which revealed that part of Michael’s brain extended down into his spinal column. This ‘Chiari malformation’ may have been contributing to his dangerous behavior, the neurologist said, and recommended surgery to fix it. Before opting for surgery, the Bolens tried giving Michael risperidone, a drug that can ease aggression and self-injury in children with autism. It helped for a few weeks, but then the effects waned. Boosting the dose restored the drug’s effects temporarily, but within five months they had reached the maximum dose.
About a year after Michael was diagnosed with the Chiari malformation, he underwent a three-and-a-half-hour procedure to remove a small piece of his skull and a piece of a vertebra to ease the pressure on his brain. At the same time, the surgeon repaired a portion of his dura, the outermost layer of the meninges. Dura should be tough, but the surgeon reported that Michael’s, for some reason, had the consistency of wet newspaper.
Even so, the surgery seemed to go well. Within 24 hours, though, Michael developed meningitis, a rare infection of the meninges. He recovered, but 10 weeks after the surgery, he began to have seizures. At first, they were sporadic, but within two years Michael was having a severe seizure every week. He would suddenly stop moving and then slowly begin to circle the room in a trance-like state. His lips would sometimes turn blue, signaling a lack of oxygen. Doctors suggested giving him Diastat (diazepam) — an anticonvulsant drug — if a seizure lasted more than five minutes. Even with the medication on hand, his mother sometimes panicked and called 911.
In June 2014, when Michael was 13 years old, he had his first convulsive seizure. His father was just drying him off after a shower when his 180-pound body went limp. His parents realized they could no longer keep him safe at home. That October, Michael moved into a residential facility in Media, Pennsylvania, a 10-minute drive from their house. Michael had his final seizure 18 months later.
When Michael died, Bolen’s Google search led her to Autism BrainNet, a network of brain banks set up in 2014 to preserve the brains of people with autism for research. (Autism BrainNet is funded by the Simons Foundation, Spectrum’s parent organization.) She called the network’s main number, and the organization worked with a local agency to collect Michael’s brain and ship it to Hof’s lab at Mount Sinai.
”“If you want to look for neuropathology in these brains, you're going to need numbers.” Patrick Hof
Brain power:
B
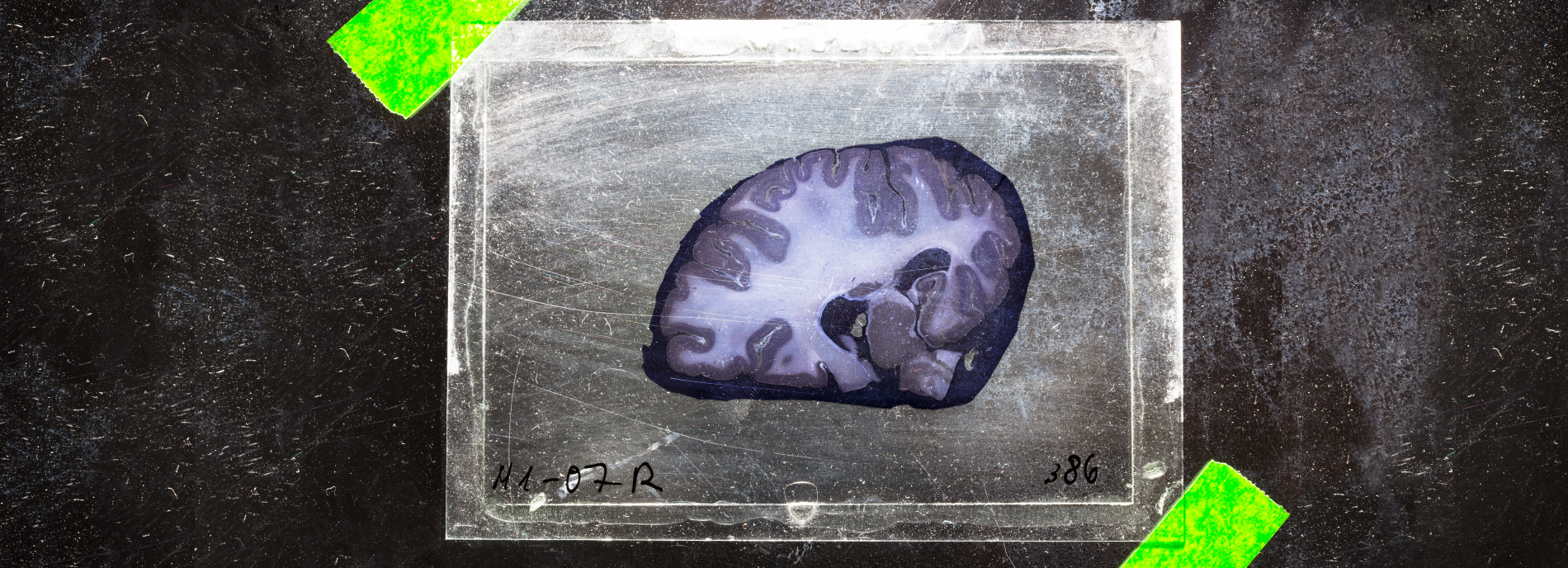
rain banking is a finely tuned science, aimed at maximizing the research potential of each precious sample. Each brain is first dissected into its two halves, or hemispheres. One hemisphere is then cut into slabs about 1 centimeter thick; the slabs are quickly frozen in liquid nitrogen and stored in labeled bags. These can be kept in a deep freezer for years, if not decades.The other hemisphere is typically submerged in a pungent formaldehyde bath that hardens the tissue and fixes each cell in place. Some brain banks keep this fixed hemisphere whole. Others cut it into slabs of tissue, also about a centimeter thick. They can store these slabs in tubs of formaldehyde in a walk-in refrigerator or embed them in paraffin wax and maintain them at room temperature. They can later shave the waxed blocks into delicate slices for inspection under a microscope as needed.
Imaging studies can provide clues to when and where brain development is altered in autism, but only postmortem tissue can reveal how development goes awry. “You have to be looking at the individual cells in those brain regions that appear to be developing differently,” says Cynthia Schumann, associate professor of psychiatry and behavioral sciences at the University of California, Davis MIND Institute.
One of the first autism studies of postmortem brain tissue, published in 1986, analyzed tissue from four males with the condition, ranging in age from 10 to 22 years. The researchers focused on the cerebellum — a wrinkly lobe at the back of the brain that helps to coordinate movement, among other things — and found a dearth of a type of neuron called Purkinje cells. The results prompted Courchesne to wonder whether the same feature would be visible in brain scans from people with autism. Using magnetic resonance imaging (MRI), he confirmed in 2001 that a worm-like structure known as the cerebellar vermis, which is normally rich in Purkinje cells, is smaller in people with autism than in controls.
Courchesne also showed that young boys with autism have an unusually large prefrontal cortex — a brain region involved in attention, decision-making and social behavior. The scans hinted at an early overgrowth of neurons in the prefrontal cortex. To confirm this, his team manually counted neurons in samples of brain tissue from seven boys with autism and six controls. They discovered in 2011 that the boys with autism had, on average, 67 percent more neurons in the prefrontal cortex. “We were astonished,” Courchesne recalls. Neurons in the prefrontal cortex develop during the first and second trimesters of pregnancy, so the findings provided some of the first evidence that autism originates before birth.
Brain tissue has also shed light on which genes are involved in autism. A 2011 study found, for example, that brains from people with autism show an increased expression of immune genes and diminished expression of genes involved in neuronal connections. A 2014 study with more brains, including some used in the 2011 study, confirmed these findings. The team behind the first study later discovered that people with classic autism share patterns of brain gene expression with those who have dup15q duplication syndrome — a rare genetic condition associated with autism. In a separate study, they showed that the brains of people with classic autism and those with dup15q syndrome bear a similar pattern of chemical tags that affect gene expression.
Together, the studies hint at a common molecular signature across multiple forms of autism, regardless of the cause or clinical features. “I don’t think we would have been able to find that result without looking at gene expression in autistic brains,” says Dan Arking, associate professor of medicine at Johns Hopkins University in Baltimore, who led the 2014 study.

Net effect:
T
he tissue for Arking’s analysis came from two brain banks: one in Maryland that is now part of the NeuroBioBank, and the one at Harvard University. Arking says he could tell the Harvard tissue was of poorer quality, thanks to quality-control steps he included in his analysis. “We could, based on our data, go back and identify which brain bank the samples came from,” Arking says. He suspects the Harvard freezer may have been warming for months, explaining the low quality of some of the specimens they had received.Two years after the freezer malfunction, in 2014, several nonprofit organizations came together to form Autism BrainNet. The idea had been in the works before the malfunction but quickly gained momentum, says David Amaral, director of Autism BrainNet and distinguished professor of psychiatry at the MIND Institute. (Autism BrainNet was jointly funded by the Simons Foundation and Autism Speaks initially, but the Simons Foundation became its sole funder in 2016. Another nonprofit organization, the Autism Science Foundation, coordinates outreach.)
Autism BrainNet has 164 autism brains from the Autism Tissue Program. As of October, it has collected an additional 41 autism brains, 56 control brains and 13 brains from people with other genetic conditions, including dup15q syndrome. It has five collection ‘nodes’ — teams trained to process brain tissue — that partner with local hospitals, organ procurement programs and medical examiners, who each raise the possibility of brain donation with grieving families. To reach families earlier, the program runs a campaign called “It Takes Brains.” Families can register regardless of whether any members have an autism diagnosis because having control brains is important for research. Autism BrainNet also works closely with advocacy groups for related syndromes.
“We’re all hoping to find a common cell-system defect,” says Carol Tamminga, chair of psychiatry at the University of Texas Southwestern in Dallas and director of the Texas node of Autism BrainNet. Finding that common alteration could point to treatments for multiple types of autism, which is most families’ primary motivation for donating brains. “They mourn their family member’s passing, for sure, but they want to think that that life will also be useful in helping other people,” she says.
Jeanine and Bill Rossbach heard about Autism BrainNet through the Dup15q Alliance. Their son, Michael, began having seizures at 7 months and was diagnosed with dup15q syndrome around his second birthday. He didn’t receive a formal autism diagnosis until he was 15, but his mother — a special-education teacher — had suspected it since he was an infant. The Rossbachs constantly worried about his safety. Michael would sometimes bolt, or ‘elope,’ out the door, and he had excruciating gut pain that would make him bite his hands until they bled. His digestive problems made him small and frail. His body seemed to weaken with every seizure and his related health issues intensified before his death at age 35.
One morning in December 2015, Michael’s father opened the door to his bedroom and found him lying, as he usually did, on his side with his head resting on his right arm. “He must have died probably no later than midnight,” Bill Rossbach recalls.
The Rossbachs knew they wanted to donate their son’s brain, but time was of the essence. The family’s home in Acme, Michigan, was nowhere near a brain bank. Jeanine Rossbach called Autism BrainNet, kicking off the search for someone who could harvest Michael’s brain. Eventually, BrainNet found someone in Wisconsin willing to make the four-and-a-half-hour drive over the upper peninsula of Michigan in the snow to collect Michael’s brain and arrange for its delivery to Mount Sinai. “I’m forever grateful,” Jeanine Rossbach says. “I wanted to make his life as meaningful to others as possible.”
”“We are simply limited by the number of brains available.” Cynthia Schumann
Limited resource:
T
he Netherlands Brain Bank launched a campaign with the slogan “We need brains” last year, encouraging people with a range of psychiatric conditions to register as brain donors. As of October, 179 adults with autism have registered to donate their brains, according to Mignon de Goeij, who manages the Netherlands Brain Bank in Amsterdam. But the bank has yet to collect an autism brain. “It’s the only disorder we have tried to collect [for] that we haven’t gotten a brain [for] yet,” says de Goeij. More than half of the registrants with autism were born after 1970, so brain donation is still years away for many of them, she says.As of October, more than 4,000 people are registered donors with Autism BrainNet. John, a 54-year-old man with autism who lives in Connecticut, registered last year. He learned about the initiative through a lawyer who helped him write his will. His job in the power industry is extremely dangerous. (He requested that we use only his first name because his employers do not know he is on the spectrum.) He says he wants to know that if he dies on the job, his organs and brain will go to good use. John has already donated 13 gallons of blood to the American Red Cross — enough to fill his own body about eight times. Donating his brain, he says, “goes right along with that.”
Autism BrainNet’s growing collection will be available to researchers in 2018, Amaral says. A panel of experts will review each request for tissue, considering its scientific merits and the type of tissue available. Some brain regions are large, and there is plenty of tissue to go around; others are quite small, and competition for those tissues is fierce. The fusiform face area, for instance, occupies a piece of the brain’s surface no bigger than a chickpea. Hof and his team have found a shortage of neurons in this area in people with autism. The difference in neuron number between autism and control brains is subtle, he says. “You can find it, but you have to look for it; it’s little bit of a needle-in-a-haystack search.”
Another brain region, the amygdala, is about the size of an almond and helps to process emotions, a function altered in people with autism. A 2006 study by Amaral and Schumann that looked at 9 autism brains and 10 control brains revealed a decrease in neurons in the amygdalae of people with autism. But subsequent analyses with 31 more brains have painted a more complex picture: Adults with autism have a dearth of neurons in the amygdala, but children with the condition have a surplus. The findings have yet to be published, but they reinforce the need for more postmortem brains. “To this point, all studies of the autistic brain have been underpowered,” Amaral says.
To help boost the studies’ power even with limited samples, Amaral and others are developing a new method to process the tissue. Instead of storing the fixed hemisphere whole, they plan to slice it into about 2,000 paper-thin sections that can be rolled up like scrolls and stored in fluid-filled test tubes. They can then cut these sections further to isolate certain brain regions, or slice them for various types of microscopy. That way, a single brain region the size of the amygdala could be cut into 215 sections that multiple labs can then use.
The brain banks also collect clinical data for every brain donor — including diagnostic records, brain scans and genetic sequences. In addition, the clinical coordinator from Autism BrainNet visits each donor’s family and interviews the members to piece together a detailed portrait of the deceased person’s clinical profile. Collecting these data could help to cut through autism’s heterogeneity problem: A string of studies over the past three years have shown, for example, that some mutations linked to the condition affect only a subset of a person’s cells. The proportion of brain cells affected, and where they are in the brain, may influence the type and severity of the person’s condition.

A host of new techniques is making it possible to analyze gene expression in individual cells from postmortem tissue. “There is some really exciting research and techniques available now; we are simply limited by the number of brains available,” Schumann says. She notes that one brain donated before Autism BrainNet launched has already been used in more than 30 studies. “Every single donation makes a big difference.”
The researchers who study donated brain tissue understand the sacrifices families have made. “We do appreciate that our success is based on a family having to go through a really difficult time,” Amaral says. “Knowing that, we try to do everything in our power to make it as straightforward and easy as possible for families to make a donation.”
Hope that something good will come of her son’s brain donation is the only thing that brings Leslie Bolen comfort. Bolen wears a heart-shaped locket that is etched with Michael’s fingerprint and contains a pinch of his ashes. Advocating for Michael was her full-time job for 14 years. In a way, donating his brain lets her continue that work, helping children like her son.
Bolen had one request when she made the donation: She wanted to see Michael’s brain at the bank and keep a photograph of it. It’s not something many parents request, and even her husband, Chad, didn’t feel he could accompany her. But the clinical coordinator connected Bolen with Hof to make the arrangement. “[Hof] was just so warm and understanding and empathetic,” Bolen says. “He knew where I was coming from.”
Bolen got to visit Hof’s lab in New York City twice. She held Michael’s brain in her hand. And felt at peace.
Syndication
This article was republished in The Atlantic.
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter

Smell studies often use unnaturally high odor concentrations, analysis reveals

‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt
