Inside every nerve cell is a complex web of protein filaments and tiny tubules that gives the cells their structure and mobility. This cytoskeleton plays a vital role in the formation of the central nervous system during embryonic development, and a growing body of evidence has linked neurodevelopmental conditions to differences in the form and function of this cellular scaffolding.
Several genes related to autism and intellectual disability, for example, are known to help regulate the cytoskeleton. In March, a study conducted in a mouse model of fragile X syndrome, the most common inherited form of autism, convincingly linked cytoskeletal alterations in the brain’s striatum to inflexible behavior on learning tasks. Cognitive inflexibility is a common characteristic of people with fragile X and autism more generally.
Intriguingly, the study — which explored the dysregulation of actin, a key cytoskeletal protein — also found that this inflexibility improved if the researchers gave the mice an activated enzyme to correct actin regulation.
“We put a molecular signature on a key autism trait,” says lead investigator Claudia Bagni, professor of fundamental neurosciences at the University of Lausanne in Switzerland.
Although scientists have long known that actin remodeling shapes synaptic plasticity, Bagni’s findings support the idea that autism and other neurodevelopmental conditions are associated with differences in this cytoskeletal molecule, Bagni says. “It seems that actin is front and center.”
The findings also suggest that a better understanding of the role of cytoskeletal proteins in autism could open the door to new interventions. But achieving that understanding remains a challenge.
“A lot of proteins involved in cytoskeleton modulation also have roles in cellular metabolism, so it’s hard to nail everything down to one pathway,” says Froylan Calderón de Anda, head of the Neuronal Development Research Group at the University Medical Center Hamburg-Eppendorf in Germany. “But we can certainly say that problems in cytoskeletal modulation may lead to neurodevelopmental conditions such as autism.”
T
he cytoskeleton is made of a network of filaments that constantly grow, shrink, attach and detach from one another, providing the mechanical support neurons need to divide, move and form new synaptic connections. The filaments can also act as railroad tracks, helping cargo move to and from different parts of the cell.In stem cells derived from autistic children, the polymerization of actin molecules into such filaments is altered, according to a 2018 study. The findings “weren’t surprising,” given the role of these filaments in steering neurodevelopment, says lead investigator Karina Griesi Oliveira, head of the Neurology Research Group at the Hospital Israelita Albert Einstein in São Paulo, Brazil. But, she adds, “it was surprising that only a few autism researchers were looking at the cytoskeleton.”
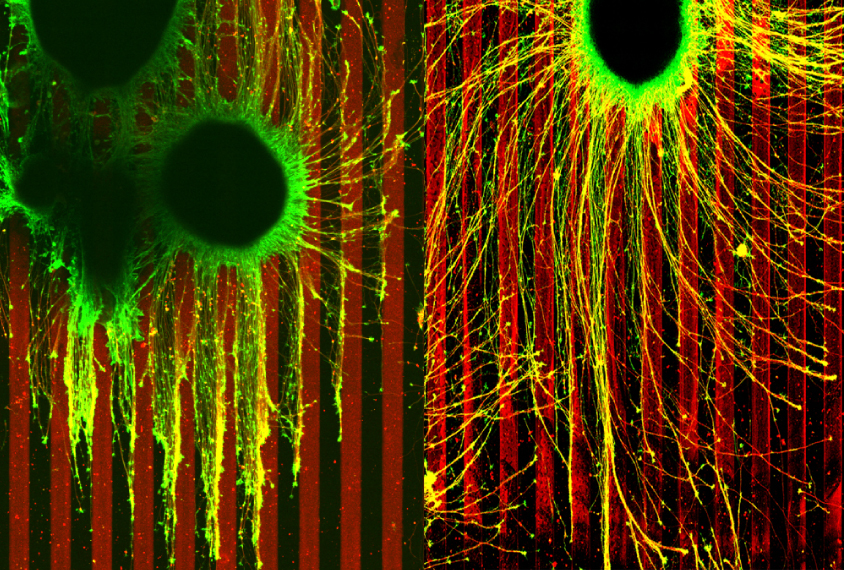
Since then, more links between the cell’s skeleton and neurodevelopmental conditions have emerged. Intellectual disability and autism have been associated with mutations in PAK1, an enzyme that is activated by a family of enzymes called Rho GTPases, which regulate actin and other structural molecules. Also, an enzyme called RhoA is overactive in lab-grown organoids derived from the brains of people with deletions or duplications in 16p11.2, a chromosomal region associated with autism, according to a 2021 study. Dampening the protein’s activity in the organoids rescued defects in neuronal migration, the study found.
RhoA has also been tied to the overgrowth of axons in neurons lacking one copy of TSC2, a gene implicated in an autism-related condition called tuberous sclerosis. Axons from such neurons grow uncontrollably, ignoring chemical signals that are known to control brain wiring, a 2021 study showed.
“If the cytoskeleton or its regulation is disrupted in some way, axons aren’t going to be guided properly and won’t make the proper connections,” says Timothy Gómez, professor of neuroscience at the University of Wisconsin-Madison, who led the study.
B
eyond helping neurons migrate, the cytoskeleton also supports their communication.Scientists have known that the SHANK3 gene, which is mutated in 1 to 2 percent of people with autism, codes for a protein that binds to actin filaments in dendritic spines — small protrusions on the neuronal surface that form synapses with other neurons. Compared with controls, mice that lack SHANK3 have fewer dendritic spines and show less frequent spontaneous excitatory postsynaptic currents in the striatum, a brain region involved in processing social reward. Behaviorally, the SHANK3-deficient mice engage in repetitive grooming and show deficits in social interaction.
Reduced actin turnover in the striatum of fragile X mice results in immature, malformed dendritic spines — a feature of both autism and fragile X syndrome, according to Bagni’s latest work. In standard behavioral tasks, the mice have trouble adapting to changing circumstances. Restoring actin dynamics in the striatum rescues the dendritic spine defects and improves the animals’ behavioral flexibility, the researchers found — evidence that problems with cytoskeletal actin caused both.
Such discoveries linking specific changes in the cell’s skeleton to traits associated with autism may yield not only more clues about the mechanisms behind the condition, but potential targets for therapies, says Pirta Hotulainen, head of the Cellular Neuroscience Research Group at the Minerva Foundation Institute for Medical Research in Helsinki, Finland, who did not take part in the study.
Manipulating actin could be risky, however, because the protein is found in every cell of the body, Hotulainen cautions. “The key would be to find actin-regulating proteins that are involved only in specific processes — for example, in synaptic plasticity.”
A
ltered actin dynamics may not be the only cytoskeletal difference leading to changes in brain structure and function. An analysis done in frog embryos, which was posted as a preprint earlier this year, found that five known autism-linked genes localize to microtubules — cytoskeletal components that are essential for cell division and movement. One protein variant of TAOK2, a gene located in the 16p11.2 chromosomal region, also binds to microtubules, a study published last year showed. Boosting the expression of this protein variant in mice missing TAOK2 rescues defects in neuronal movement during embryonic development, the researchers found.The findings may explain why people with 16p11.2 deletion syndrome, nearly one-third of whom have autism, have a thinner cerebral cortex than neurotypical people do, says Calderón de Anda, who led the study. “If neurons are not migrating properly during development, they end up in the wrong layer and this leads to connectivity issues later on.”
Microtubules also form the core structure of cilia — thin protrusions on a cell’s surface that sense its external environment and signal to the cell to respond. Defects in cilia have been tied to fragile X syndrome, tuberous sclerosis and autism. In the brain, cilia on the surface of neurons can form synapses with the axons of other neurons, researchers reported last year. And the activation of these cilia-axon synapses, the work also showed, can ultimately alter chromatin, the DNA-protein complex that helps to regulate gene expression.
This connection means that cytoskeletal alterations could, in theory, hinder gene expression during brain development, leading to differences in neural circuitry and activity, says study investigator Shu-Hsien Sheu, a senior scientist in David Clapham’s lab at the Janelia Research Campus in Ashburn, Virginia.
The findings, Sheu says, “open the door to many more questions” about the role of the cell’s skeleton in autism.





