Autism studies hampered by lack of reliable test for gut problems
Experts from various fields should work with parents to develop a standardized questionnaire for gut problems in people with autism.

In his first description of autism in 1943, Leo Kanner described children with social problems, repetitive behaviors and language difficulties. But one more feature in his description would become a mainstay of autism: gastrointestinal distress1,2.
Since his report was published, dozens of studies have documented gastrointestinal issues, such as constipation, diarrhea and abdominal pain, in people with autism.
By some estimates, more than 70 percent of people with autism have gastrointestinal issues. But other studies have pegged the prevalence as low as 9 percent3. We suspect these discrepancies are in part due to the way gastrointestinal problems are measured4,5.
Although there are good tools for assessing gastrointestinal problems in clinical practice, there are no reliable tools for use in epidemiologic studies. For these studies, we need questionnaires that a participant or caregiver can complete outside of a doctor’s office.
Not even the tools doctors use have been adapted for individuals with autism, who may have difficulty communicating. Some clinicians use parent reports to gauge gastrointestinal symptoms in children. But parents may not always know their child has abdominal cramps or discomfort, and may instead think that behavioral outbursts rooted in pain are just manifestations of autism.
Even if clinical or epidemiological tools can capture certain gastrointestinal symptoms in people with autism, not all of them include questions about diet, mealtime behaviors and other autism-related behaviors, such as aggression and self-injury. These behaviors may signal gut problems in a person who has difficulty communicating. In short, we just don’t know if these tools are measuring what we think they are in people with autism.
The ability to accurately measure gastrointestinal symptoms in people with autism is critically important for several reasons. It could reveal whether certain treatments cause or exacerbate them. It could also tell us whether they are linked to certain risk factors for autism, such as maternal immune activation, or whether gut health itself is a risk factor for autism. And it could reveal whether treating the symptoms can ease autism-related behaviors.
We examined how researchers assess gut problems in autism and how their results vary with the methods they use. We found the severity and frequency of the problems vary greatly across studies and that much of the variation is due to differences in how data is obtained.
Gut feeling:
To see how researchers test for these problems in autism, we searched back to 1980 for any paper on autism that includes measurements of the symptoms. We found 144 studies. We homed in on 84 studies that did not include or exclude participants based on gastrointestinal symptoms or diet.
We calculated the median frequency of specific symptoms across the studies, and then carried out statistical analyses to determine whether the frequency of specific symptoms depends on the characteristics of the study’s participants or its methodology.
We found that the frequency of symptoms varies dramatically across studies. For example, the proportion of people with constipation ranges from 4 to 46 percent, and the rate of diarrhea ranges from 2 to 76 percent6.
The studies also vary in who reported the symptoms — whether it was a parent, teacher, physician or individual with autism. Interestingly, studies that do not specify who reported the symptoms tend to report the most severe ones. Studies that use medical records or claims data report the highest frequency of reflux symptoms. And studies based in clinics or involving individuals at high risk for autism have the highest frequency of constipation.
The frequency of symptoms also depends on the age of the individuals with autism: Studies of individuals with a mean age of 13 to 18 years report a higher frequency of abdominal pain and reflux than those involving younger children. This makes sense given that older children are likely to be better able to report more nuanced symptoms, such as pain and the sensation of reflux, than are younger children.
Team effort:
Our findings highlight the need for a standardized tool to assess gastrointestinal problems in autism. We believe this tool should be a questionnaire that parents or caregivers complete, especially when an individual is nonverbal, so it can be implemented in large epidemiologic studies.
A team of experts in gastroenterology, pain, feeding, autism and questionnaire development should work together to develop the tool. Individuals with autism and their parents should also be involved in this process.
It is important that the tool includes questions about diet, such as whether an individual avoids certain types of foods based on texture, color, temperature or taste. It should also ask about behaviors at mealtime, such as self-injurious actions or aggression; and possible reactions to gut pain, such as grimacing or applying pressure to the abdomen.
Some individuals may limit their diet because of gastrointestinal symptoms caused by certain foods. Alternatively, restrictive dietary preferences may lead to problems. Behaviors at and away from the table may be a response to gut symptoms and pain.
Until this tool is developed, studies of autism should clearly describe how gastrointestinal symptoms were measured. They should state which questionnaire was used, who reported the symptoms, and other important characteristics, such as the age and race of the participants.
Demographic characteristics may be linked to gastrointestinal symptoms, so this information can help researchers, clinicians and families interpret the findings of studies. Individuals with autism, their families and the quality of research will all benefit from a standard, valid approach to measuring these symptoms in this population.
Daniele Fallin is professor and chair of the mental health department at Johns Hopkins University’s Bloomberg School of Public Health and director of the Wendy Klag Center for Autism and Developmental Disabilities. Calliope Holingue is a graduate student in Fallin’s lab.
References:
- Kanner L. Acta Paedopsychiatr. 35, 100-136 (1968) PubMed
- Bresnahan M. et al. JAMA Psychiatry 72, 466-474 (2015) PubMed
- Buie T. et al. Pediatrics 125, S1-18 (2010) PubMed
- Coury D.L. et al. Pediatrics 130, S160-168 (2012) PubMed
- van den Berg M.M. et al. Am. J. Gastroenterol. 101, 2401-2409 (2006) PubMed
- Holingue C. et al. Autism Res. Epub ahead of print (2017) PubMed
Recommended reading

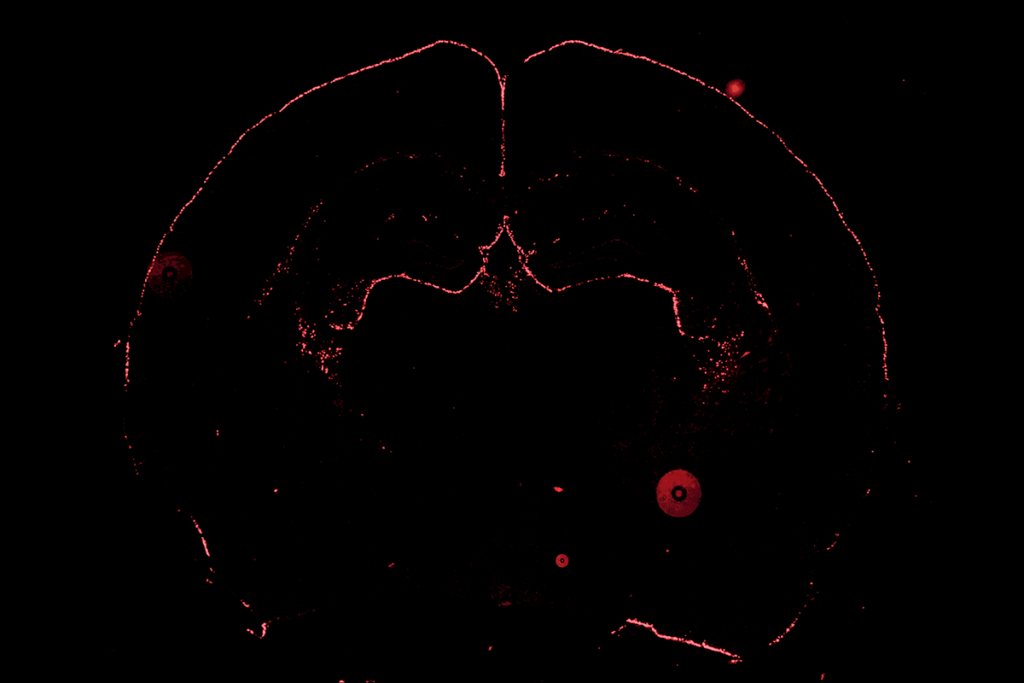
New tool may help untangle downstream effects of autism-linked genes

NIH neurodevelopmental assessment system now available as iPad app
Molecular changes after MECP2 loss may drive Rett syndrome traits
Explore more from The Transmitter
Who funds your basic neuroscience research? Help The Transmitter compile a list of funding sources

The future of neuroscience research at U.S. minority-serving institutions is in danger