The prevalence of autism in adults and children in the United States has risen over the past 12 years, new research gleaned from electronic medical records and insurance claim data shows. In particular, young adults, girls and certain racial and ethnic groups saw the greatest relative increases.
The results mirror a decades-long trend among children, as reported by the Centers for Disease Control and Prevention (CDC) in 2023. Although “many prevalence estimates to date have focused on children,” says lead investigator Luke Grosvenor, a postdoctoral research fellow at the Kaiser Permanente Northern California Division of Research, “we have a rich and large dataset here where we can also look at different age ranges, particularly adults, and describe the trends among this adult population.”
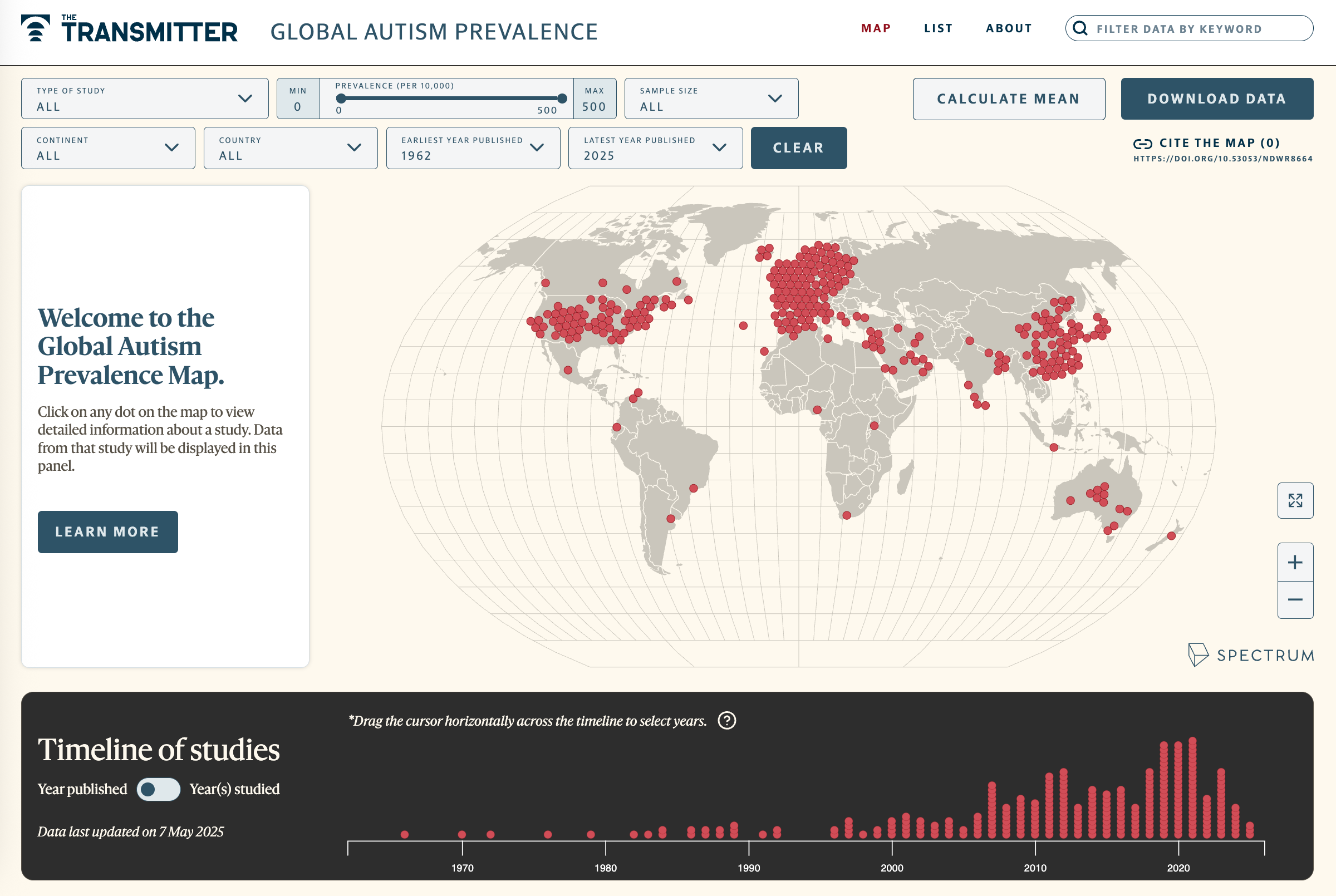
The study, published in October in JAMA Network Open, is based on data from more than 9 million people at 12 sites participating in the Mental Health Research Network across the United States. These sites are research centers within diverse health-care systems. Autistic people in this dataset were identified from International Classification of Diseases (ICD-9 and ICD-10) diagnostic codes for autism.
There’s “no perfect dataset” to look at autism prevalence says Maureen Durkin, professor of population health sciences and pediatrics at the University of Wisconsin-Madison, who was not involved in the study, but “each of these gives you an angle at it, and they’re all kind of saying the same thing,” which is that the prevalence has increased.
O
ne important finding, Grosvenor says, is a rise in prevalence from 0.7 per 1,000 in 2011 to 3.7 per 1,000 in 2022 among 26- to 34-year-olds. Although the absolute prevalence in this age range remains fairly low, this is “the group in which we saw the largest [relative] increase,” he says. “Often [it] can be a medically complex population, too, with a lot of co-occurring conditions.”
Autism prevalence also increased for both genders in children and adults over this time period, but relative increases in girls were higher than in boys: 305 percent compared with 185 percent, respectively. That represents “a little bit of a narrowing of the ratio of diagnosis in males to females,” Durkin says, but “it's still in that range of roughly three times more males than females being diagnosed.”
Among children, race and ethnicity patterns are consistent with CDC data, Grosvenor says. “We're seeing increases in prevalence in non-white populations,” particularly in children, he says. That finding could mean disparities in screening and diagnosis are decreasing. Prevalence is highest among American Indian and Alaska Native children and adults, the authors write, which has not been previously reported in adults. (The term “American Indian” is not in keeping with The Transmitter’s house style but reflects the terminology used in the study, which is based on the official U.S. census designation.)
The investigators have interpreted the race and ethnicity data with appropriate nuance, says Mayada Elsabbagh, professor in neurology and neurosurgery at McGill University, who was not involved in the study. In the case of American Indian and Alaska Native populations, she says, the numbers could reflect “the characteristics of the sites where the data is being collected.” The authors note that perhaps proximity or partnerships between the health-care facilities and Native communities could be driving this specific pattern.
Often researchers attempt to explain these kinds of group-level findings by invoking biology, Elsabbagh says, although “we just don't have evidence to back that up.”
Eric Fombonne, professor emeritus of psychiatry at Oregon Health & Science University, who did not contribute to this research, wrote in an email that a limitation of this analysis is that the prevalence reported is “underestimating the population prevalence,” given the study’s focus on describing the total number of people with an autism diagnosis in a particular health-care system.
Indeed, Grosvenor points out, this study was not designed to tease out whether the uptick reflects improved access to diagnostic services rather than a “true increase” in prevalence. “I think we cannot rule out the possibility of a true increase in prevalence. In the same sense, we can't rule out the possibility that most of this would be driven by one or more factors, including expanded developmental screening and those sorts of guidelines over the years,” Grosvenor says.
Durkin agrees: “You can't really make any inferences about causality from the data they presented. So it's more, ‘Hey, this is important. We need to be paying more attention to it.’” That includes research on possible causes, treatments and improving outcomes, she says.