Immature neurons with mutations in the autism-linked gene MYT1L fail to suppress genes that should be active only in other cell types — a shortcoming that stalls the neurons’ maturation and shifts their electrical signaling into overdrive, according to a study published today in Molecular Psychiatry.
The anticonvulsant drug lamotrigine calms the excess signaling in both human and mouse neurons and quells hyperactivity in mice with mutations in MYT1L, the study also shows.
The results are far from a guarantee that the drug will help people with such mutations, says lead investigator Moritz Mall, group leader at the Hector Institute for Translational Brain Research at DKFZ in Heidelberg, Germany. But they do begin to reveal how mutations in the gene lead to developmental delays and autism, he says. MYT1L is expressed throughout life, which “gives us a longer window of opportunity to intervene,” he says.
Fewer than 200 people have been diagnosed with MYT1L-related syndrome, which is also marked by obesity, intellectual disability and, sometimes, epilepsy. MYT1L is one of three genes needed to spur stem cells into becoming neurons. And mice with a variant of the gene have unusually small brains and prematurely developed neurons, according to a 2021 study that detailed the first mouse model of MYT1L mutations.
The new work is the first to examine how mutations in the gene affect human brain cells.
It shows that human and mouse neurons are affected similarly by MYT1L mutations, suggesting mice are a good model for studying the gene, says Joseph Dougherty, associate professor of genetics and psychiatry at Washington University in St. Louis, Missouri, and lead investigator on the 2021 study.
“That is good to see,” he says. “It means we can test therapeutics in both.”
M
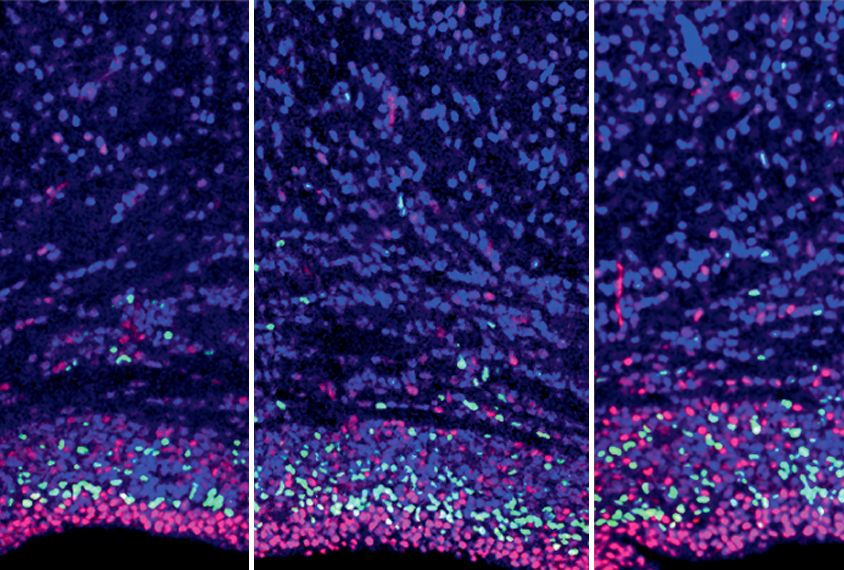
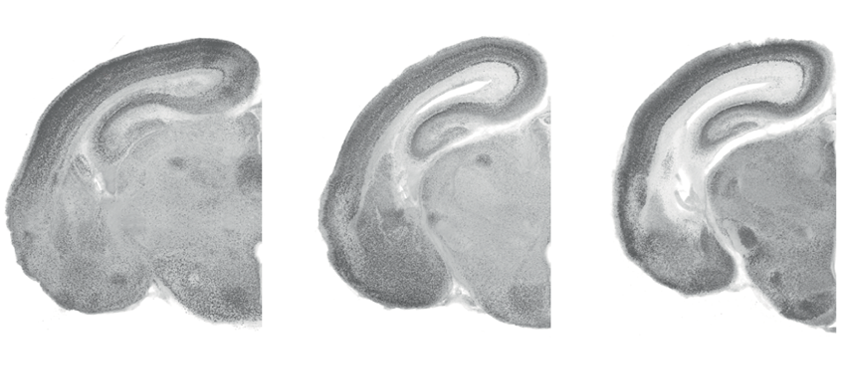
all and his team created mice with one nonfunctioning copy of MYT1L. (Mice with two mutated copies died shortly after birth.) At day 15 of gestation, the model embryos’ developing cortices had 37 percent fewer progenitor cells maturing into neurons than did the control embryos.At day 18 — just before birth — expression of genes that promote cell division remained elevated in MYT1L embryos, whereas expression of those that prompt neurogenesis was suppressed.
At birth, the cortices of MYT1L mice were 10 percent thinner than those of controls.
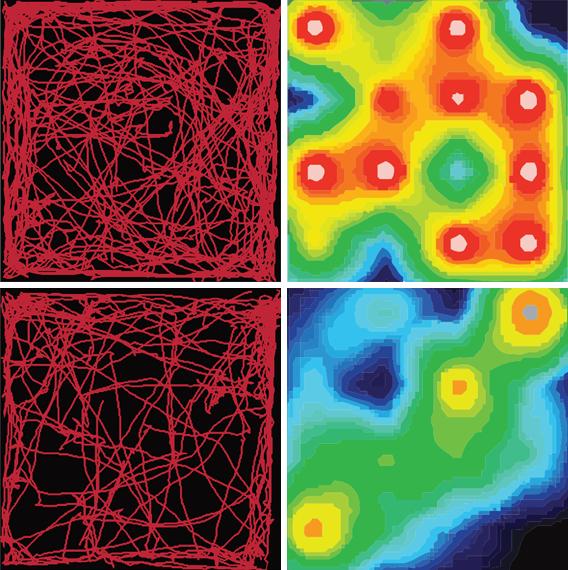
In behavioral tests, both juvenile and adult model mice were hyperactive. Male, but not female, adult mice had altered social behavior: They did not show the usual preference for a novel mouse over an unfamiliar one.
Adult model mice showed altered expression of epilepsy-, schizophrenia- and autism-linked genes, as did neurons derived from human embryonic stem cells with an MYT1L variant. Meanwhile, genes that coax cells into becoming muscle or heart tissue were active in the neurons — suggesting an “identity crisis” that delays maturation, Mall says. “The cells cannot jump from the progenitor stage that efficiently to a differentiated neural state.”
The autism-linked gene ZNF462 also represses non-neuronal genes during neurogenesis, an independent team reported in January.
H
uman and mouse neurons with MYT1L mutations showed increases in spontaneous electrical activity: In the mouse cells with just one functional copy, spikes increased an average of 400 percent.Among the genes upregulated in both mouse and human neurons was SCN5A, which encodes a sodium channel that is usually expressed in only the heart. (The related gene SCN2A, which encodes a neuronal sodium channel, is strongly linked to autism.) Knocking down SCN5A in the cells normalized their hyperactivity, as did overexpressing MYT1L.
Treating the cells with lamotrigine, which blocks sodium channels, also calmed the excitable cells, and MYT1L mice that received injections of the drug no longer showed hyperactivity or anxiety-like behaviors.
It will be important to test lamotrigine in mouse models with different mutations in MYT1L, Dougherty says.
The sodium-channel gene SCN10A, which is typically expressed in the peripheral nervous system, is active in the brain in a mouse model of Pitt-Hopkins syndrome, according to a 2016 study. It’s possible such misexpression of sodium channel genes is a “common theme” in rare autism-associated conditions, says Brady Maher, lead investigator at the Lieber Institute for Brain Development in Baltimore, Maryland, who led the 2016 work. Maher was not involved in the new study but says “it’s remarkable how similar” the mice are.
Testing lamotrigine in such genetic models could enable researchers to pool enough participants for a trial, Maher says. The drug was ineffective in a small 2001 trial of 28 autistic children, but it may help people with certain genetic conditions.
Because lamotrigine is already approved for use in people, Mall says, he plans to start a clinical trial in people with MYT1L mutations as early as next year.
“Repurposing is the way to go,” he says. “It might be a very low-hanging fruit.”