Editor’s Note
This article was originally published in June 2017. It has been revised to reflect more recent research.
The more scientists dig into DNA, the more intricate its contribution to autism seems to be. Here, we unravel the complex genetics of autism.
This article was originally published in June 2017. It has been revised to reflect more recent research.
Researchers have known that genes contribute to autism since the 1970s, when a team found that identical twins often share the condition. Since then, scientists have been racking up potential genetic culprits in autism, a process that DNA-decoding technologies have accelerated in the past decade.
As this work has progressed, scientists have unearthed a variety of types of genetic changes that can underlie autism. The more scientists dig into DNA, the more intricate its contribution to autism seems to be.
How do researchers know genes contribute to autism?
Since the first autism twin study in 1977, several teams have compared autism rates in twins and shown that autism is highly heritable. When one identical twin has autism, there is about an 80 percent chance that the other twin has it too. The corresponding rate for fraternal twins is around 40 percent.
However, genetics is not entirely responsible for a child’s chances of having autism. Environmental factors also contribute to the condition — although researchers disagree on the relative contributions of genes and environment. Some environmental influences, such as exposure to a maternal immune response in the womb or complications during birth, may work with genetic factors to produce autism or intensify its traits.
Is there such a thing as an autism gene?
Not really. There are several conditions associated with autism that stem from mutations in a single gene, including fragile X and Rett syndromes. But less than 1 percent of non-syndromic cases of autism stem from mutations in any single gene. So far, at least, there is no such thing as an ‘autism gene’ — meaning that no gene is consistently mutated in every person with autism. There also does not seem to be any gene that causes autism every time it is mutated.
Still, the list of genes implicated in autism is growing. Researchers have tallied about 100 genes they consider strongly linked to autism. Many of these genes are important for communication between neurons or control the expression of other genes.
How do these genes contribute to autism?
Changes, or mutations, in the DNA of these genes can lead to autism. Some mutations affect a single DNA base pair, or ‘letter.’ In fact, everyone has thousands of these genetic variants. A variant that is found in 1 percent or more of the population is considered ‘common’ and is called a single nucleotide polymorphism, or SNP.
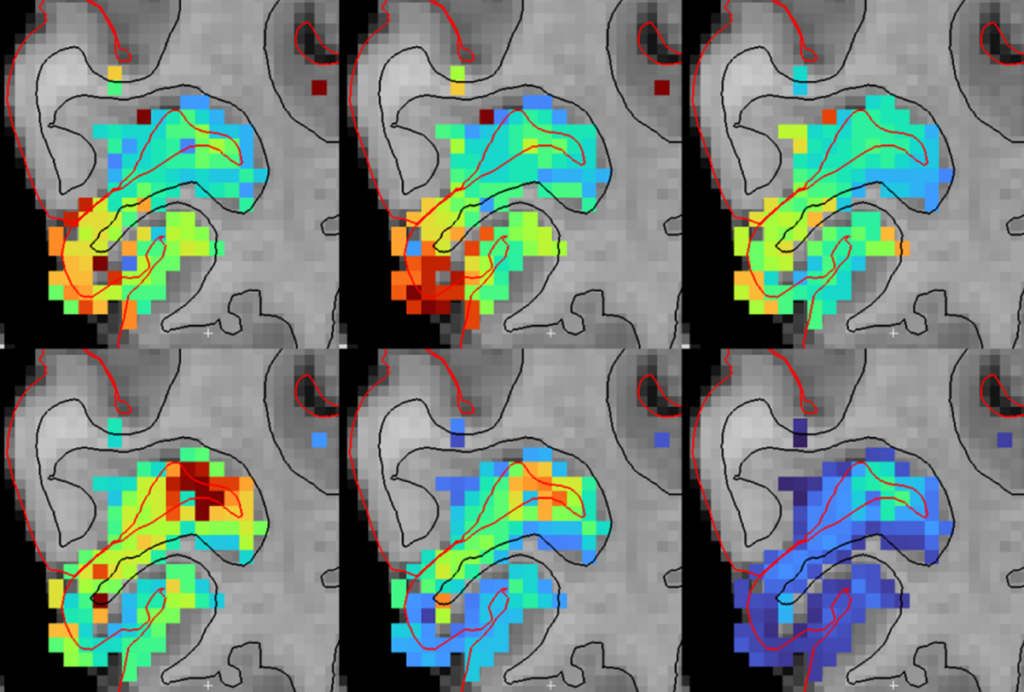
Common variants typically have subtle effects and may work together to contribute to autism. ‘Rare’ variants, which are found in less than 1 percent of people, tend to have stronger effects. Many of the mutations linked to autism so far have been rare. It is significantly more difficult to find common variants associated with autism. The largest study to date, published in 2019 and involving more than 18,000 autistic and 27,000 non-autistic people, revealed 12 regions of the genome that harbor autism-linked common variants. Two additional regions turned up in a 2020 re-analysis of the 2019 data along with about 6,000 additional samples.
Other changes, known as copy number variations (CNVs), show up as deletions or duplications of long stretches of DNA and often include many genes.
But mutations that contribute to autism are probably not all in genes, which make up less than 2 percent of the genome. Researchers are trying to wade into the remaining 98 percent of the genome to look for irregularities associated with autism. So far, these regions are poorly understood, but some evidence links autism to mutations in stretches of noncoding DNA containing regulatory elements that control gene expression.
Are all mutations equally harmful?
No. At the molecular level, the effects of mutations may differ, even among SNPs. Mutations can be either harmful or benign, depending on many cells they affect in the body and how much they alter the corresponding protein’s function. A missense mutation, for example, swaps one amino acid in the protein for another. If the substitution doesn’t significantly change the protein, it is likely to be benign. A nonsense mutation, on the other hand, inserts a ‘stop’ sign within a gene, causing protein production to halt prematurely. The resulting protein is too short and functions poorly, if at all.
How do people acquire mutations?
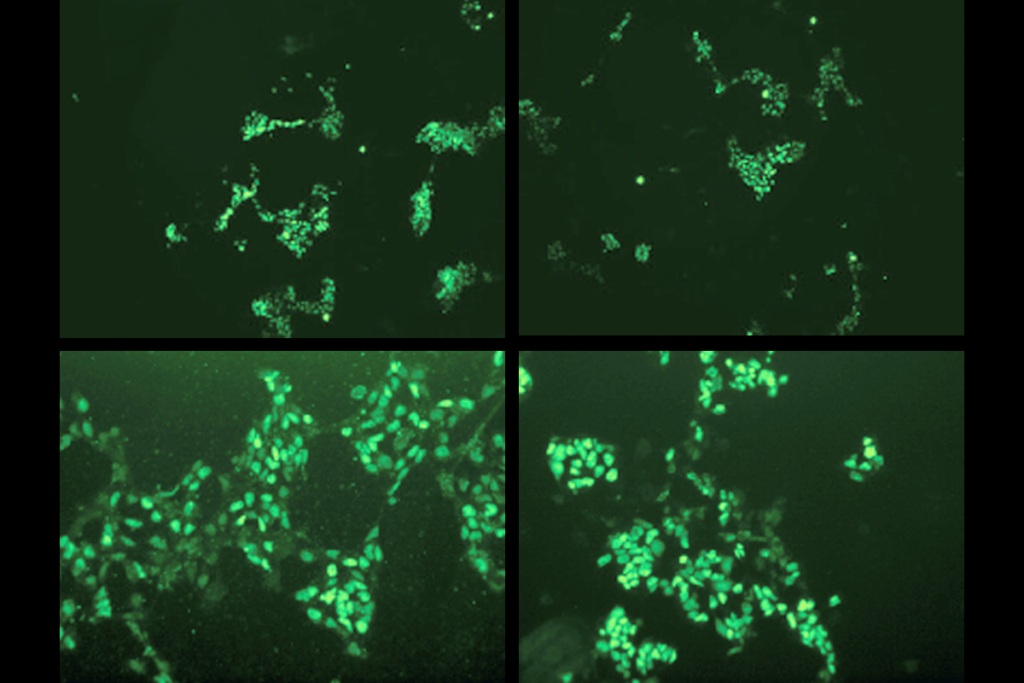
Most mutations are inherited from parents, and they can be common or rare. Mutations can also arise spontaneously in an egg or sperm, and so are found only in the child and not in her parents. Researchers can find these rare ‘de novo’ mutations by comparing the DNA sequences of people who have autism with those of their unaffected family members. Spontaneous mutations that arise after conception are usually ‘mosaic,’ meaning they affect only some of the cells in the body. The fewer cells these mutations affect, the milder their contributions to autism traits.
Can genetics explain why boys are more likely than girls to have autism?
Perhaps. Girls with autism seem to have more mutations than do boys with the condition. And boys with autism sometimes inherit their mutations from unaffected mothers. Together, these results suggest that girls may be somehow resistant to mutations that contribute to autism and need a bigger genetic hit to have the condition.
Is there a way to test for mutations before a child is born?
Clinicians routinely screen the chromosomes of a developing baby to identify large chromosomal abnormalities, including CNVs. There are prenatal genetic tests for some syndromes associated with autism, such as fragile X syndrome. But even if a developing baby has these rare mutations, there is no way to know for sure whether he will later be diagnosed with autism.
This article was republished in The Washington Post.