Autism drugs may alter brain connectivity
Children with autism who take certain medications have different patterns of brain connectivity than do unmedicated children with the condition.
Children with autism who take certain medications have different patterns of brain connectivity than do unmedicated children with the condition, a new study suggests1.
More than half of children diagnosed with autism take psychotropic drugs, such as Prozac and Ritalin, to ease features related to autism. The drugs are designed to alter brain function, so it is reasonable to assume they also affect how different parts of the brain interact.
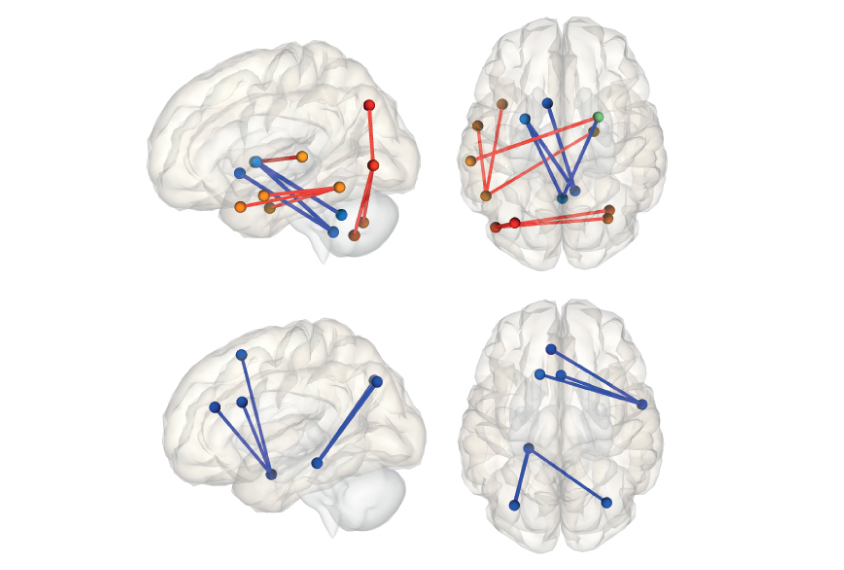
The new study hints that drug usage enhances the degree of synchronization between regions of the cortex, the brain’s outermost layer.
“Overall, there seems to be a slight effect of kids on medication showing greater connectivity,” says lead investigator Ralph-Axel Müller, professor of psychology at San Diego State University.
Researchers measure brain connectivity by looking at regions that activate in sync during functional magnetic resonance imaging (fMRI). The greater the synchrony, the more connected the regions.
Studies of functional connectivity in autism have yielded mixed results: Some suggest autism brains are more highly connected than those of controls, whereas others find evidence of decreased connectivity. The new work, published in the July issue of Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, suggests the discrepancy may arise because studies do not always control for medication use.
“It’s almost to the level of surprising that nobody has done this before,” says David Beversdorf, associate professor at the University of Missouri, who was not involved in the study.
Drug dilemma:
Müller and his team examined fMRI scans and drug information from 49 children and adolescents with autism and 50 controls. The participants ranged in age from 8 to 17 years and were matched for age, gender and head motion during the scans.
About half of the participants with autism were taking psychotropic medications, most commonly antidepressants or stimulants. These children showed greater functional connectivity between regions of the cortex than did controls. By contrast, unmedicated children showed less functional connectivity across the cortex than controls.
A direct comparison of the medicated and unmedicated groups teased out the same pattern of increased connectivity among children taking medications, but the difference is not statistically significant.
The researchers then compared scans from 14 participants with autism taking stimulants with scans from a separate group of 6 age-matched children with autism taking stimulants. The groups showed similar patterns of functional connectivity, suggesting stimulants lead to consistent shifts in connectivity patterns.
It is also possible that children with autism who take medications, perhaps because of the severity of their condition, are neurologically different from unmedicated children with autism.
“The question remains: is this a result of response to medication, or is this a result of these individuals being differently affected and thus requiring the medication? That can’t be answered [yet],” Beversdorf says.
Severity factor:
Müller and his team sought to answer that question by comparing participants with severe autism features with those with mild features, regardless of their medication status.
Children with severe repetitive behaviors — based on a subscale of the Autism Diagnostic Observation Schedule — showed decreased connectivity between cortical brain regions compared with children who have mild repetitive behaviors or controls. This finding suggests autism severity and medication use have different effects on functional connectivity.
“While there might be some relationship between symptom severity and whether they were on medication, the differences in patterns that we were seeing were not just due to symptom severity,” says Annika Linke, a postdoctoral researcher in Müller’s lab.
The findings do not mean children taking drugs should be excluded from studies, the researchers say. Other factors may also contribute to variable results from studies of functional connectivity in autism.
“It’s not a simple explanation of all the inconsistencies that we’ve had in functional connectivity MRI literature, but it is one factor that we should consider in the future,” Müller says.
Scientists should also examine the effects of dosage and the duration of treatment on functional connectivity, the researchers say.
References:
- Linke A.C. et al. Biol. Psychiatry: Cogn. Neurosci. Neuroimaging Epub ahead of print (2017) Abstract
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter

Smell studies often use unnaturally high odor concentrations, analysis reveals

‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt
