Autism diagnosis, explained
New and improved autism screens and diagnostic tools promise to streamline the long path to an autism diagnosis.
Clinicians diagnose autism using behavioral tests for the core features of the condition: communication difficulties, social challenges and restricted or repetitive behaviors.
But getting an autism diagnosis can be a long and challenging process. Because autism is a heterogeneous condition defined by behavior and not by a single gene, blood or brain profile, clinicians use reliable diagnostic tools to assess an individual’s strengths or weaknesses and develop personalized treatment plans.
However, clinicians in a given area may lack the expertise or resources needed to implement these standardized diagnostic tools. And families seeking diagnosis may face a long wait.
Some scientists are working to improve the available screening and diagnostic instruments and people’s access to them. They are also developing new diagnostic tools.
What are the standard tools for screening and diagnosing autism?
Clinicians use a range of tests to diagnose autism. Screens flag people at risk for the condition, and diagnostic tools then help clinicians determine whether a person is autistic.
The Modified Checklist for Autism in Toddlers (M-CHAT), developed in the early 1990s, is the preferred screening tool and is widely used in the United States. Parents answer 23 ‘yes-no’ questions about their child’s social, motor and language skills at the child’s 18- and 24-month checkups. A revised version of the screen includes fewer questions and a follow-up interview between the child’s caregiver and the pediatrician. Other screens, such as the Gilliam Autism Rating Scale, are used primarily in school settings and help flag children older than age 2.
To diagnose the children these screens flag, clinicians typically use a pair of standardized behavioral tests: the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R).
Clinicians using the ADOS observe children’s behavior and how they engage in social situations for up to an hour. The ADI-R is a 93-item questionnaire that caregivers complete over several hours. Clinicians sometimes also incorporate other tools that evaluate autism traits. For instance, they use the Vineland Adaptive Behavior Scales to assess daily-living skills and the Social Responsiveness Scale to identify problems with social skills.
Which tests are the most reliable?
The ADOS and ADI-R identify the greatest proportion of autistic people and make the fewest false identifications. The ADI-R has been translated into more than two dozen languages and is the preferred test among clinicians in many countries.
The M-CHAT is quick and can be widely administered, but as a screen, it only provides an indication of risk and is not always accurate. Still, versions of the M-CHAT are used in the U.S., the United Kingdom and several other countries. Researchers in China are testing a modified version of the M-CHAT as a screening tool for that country. And the revised M-CHAT with the follow-up interview is more reliable than the original questionnaire.
Which aspects of the tests are most in need of improvement?
Scientists developed diagnostic tests for autism largely using data from boys, so the tests are not as good at detecting autism in girls. Autism is also underdiagnosed among minorities and children from low-income families, although it’s unclear whether existing diagnostic tools contribute to the disparity.
Some tools work better at certain ages than at other ages. For instance, three 2017 studies indicate that the M-CHAT is more accurate when conducted at 24 months of age than at 18 months. It fails to spot children with the condition at 18 months — and wrongly flags others as having autism. One study showed that only 36 percent of children in this age group whom the revised M-CHAT flags for autism actually have the condition1.
What other factors hinder autism diagnosis?
Autism can be diagnosed by age 2, but early screening isn’t universal, and some children aren’t flagged until they begin preschool — or even much later.
One of the biggest barriers to early diagnosis is a dearth of trained clinicians. Doctors need significant clinical expertise to administer the ADOS and the ADI-R, so many forego these instruments in favor of shorter, less rigorous tests2. What’s more, pursuing a diagnosis can also be costly and time-intensive for families that live far from an expert clinician.
What new tools are on the horizon?
Many teams are looking for biomarkers of autism — objective biological signatures of the condition. Some are using eye-tracking technology to assess what autistic people pay attention to; several studies show that autistic people tend to avoid others’ eyes, preferring instead to look at their mouths or at scenery. Eye-tracking can even reveal telltale patterns of focus in infants, but it is still a long way from being ready for use in the clinic.
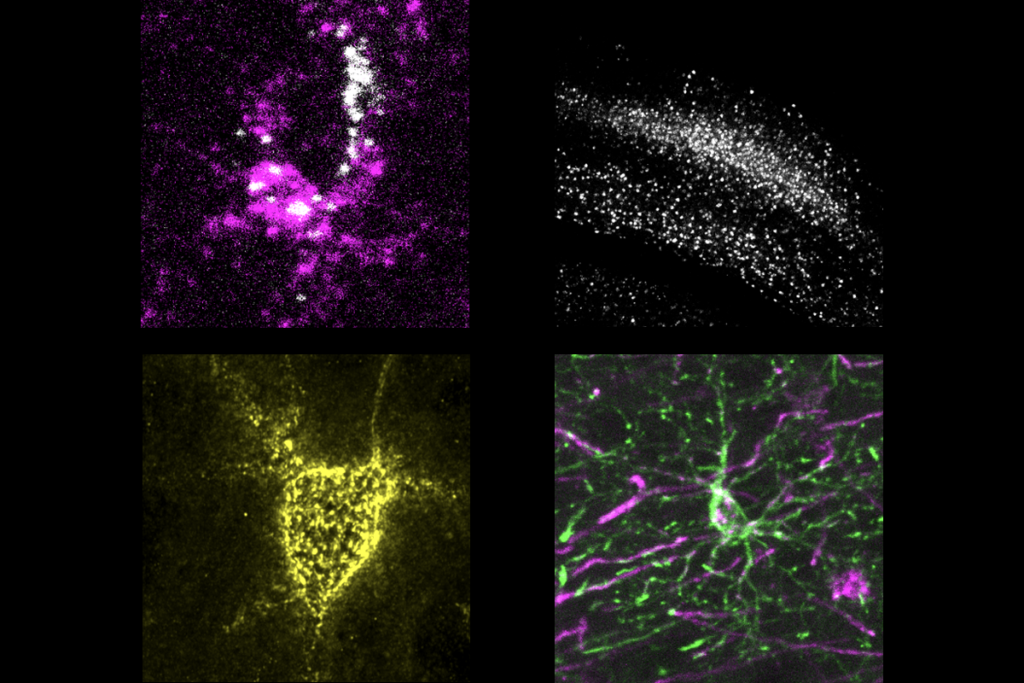
Heart rate, sleep patterns and body movements may serve as biomarkers, too. And researchers are looking for brain signatures of autism by using technologies such as magnetic resonance imaging. Machine-learning tools may aid in the analysis of these biomarkers. Genetic testing could also inform diagnosis: A long list of genes is implicated in autism.
Some of these tools face practical barriers. Broad clinical use of brain scanning is prohibitively expensive, for example, and genetic testing can be costly for families when it isn’t covered by insurance.
Meanwhile, some teams are developing behavioral screens that identify autism in infants; others have found ways to reach parents in the U.S. with limited English skills3.
The next phase of behavioral instruments may characterize a person’s autistic features enough to identify subtypes of autism — and develop targeted treatments based on these profiles.
References:
Recommended reading
Explore more from The Transmitter

Neuro’s ark: How goats can model neurodegeneration