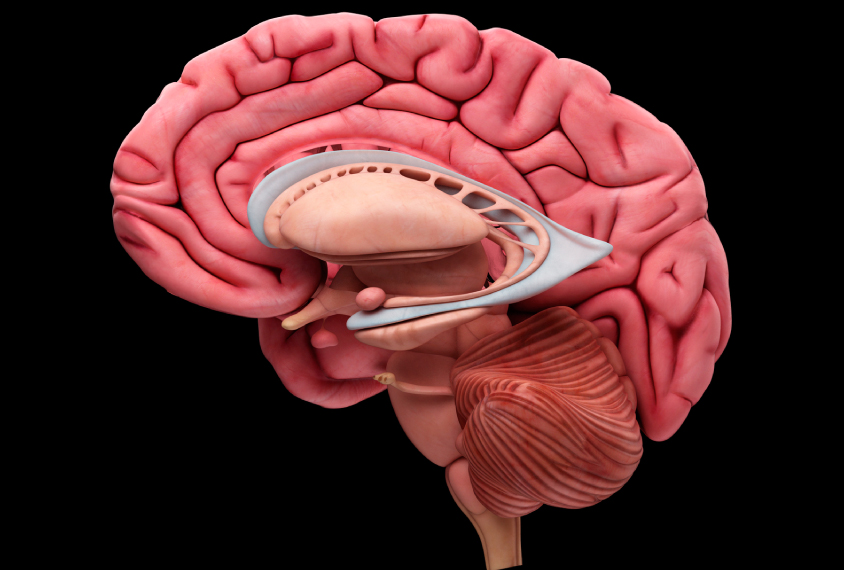
In autism, brain’s emotion hub begins with too many cells
The amygdala, a brain region that governs emotions, may be enlarged and overly connected in children with autism, but it shrinks as the children grow up.
Editor’s Note
This article was originally published 13 November 2016, based on preliminary data presented at the 2016 Society for Neuroscience annual meeting in San Diego, California. We have updated the article following publication of the work on 3 April in Proceedings of the National Academy of Sciences and 1 February in the Journal of Computational Neurology2,3. Updates appear below in brackets.
The amygdala, a brain region that governs emotions, may contain an unusually high number of neurons in young children with autism. Each of these neurons may also have an excess of connections to other cells. As these children grow up, however, some amygdala neurons, and many of their connections, seem to disappear.
The unpublished findings, which come from two postmortem brain studies, were presented yesterday at the 2016 Society for Neuroscience annual meeting in San Diego.
The data mesh with those of brain imaging studies showing that an enlarged amygdala in children with autism gradually assumes a typical size as they get older1. Researchers have seen a similar trend for overall head size in autism.
The findings may shed light on the mechanisms behind broader changes in brain size and connectivity seen in imaging studies, says Cynthia Schumann, associate professor of psychiatry and behavioral sciences at the University of California, Davis, and lead researcher on both studies. “It’s really leading to this idea that we have somehow an excess [of cells and connections] in autism brains, and we are finding it everywhere we look,” she says.
In the first study, the researchers looked at postmortem brains from 28 individuals with autism and [24] controls who ranged from 2 to 48 years old. In typical individuals, the number of neurons in the amygdala increases by an average of [11] percent [from youth to adulthood], the researchers found2. [The researchers looked at trends across the participants rather than tracking changes in individuals over time.]
[Adults with autism, by contrast, have roughly 17 percent fewer neurons than children with autism do, the team found.] Children with autism show an average of [11] percent more neurons than typically developing individuals during early childhood. But the number of neurons declines over time, so that by adulthood, the brains of people with autism have [roughly 20 percent] fewer neurons in the amygdala than do those of controls.
Preliminary data suggest that the increase in amygdala neurons in typical individuals may stem from a pool of developing neurons that sit at the border of the amygdala and a neighboring brain region called the paralaminar nucleus, says Thomas Avino, a postdoctoral fellow in Schumann’s lab, who presented the findings. These immature neurons are abundant in the brain of a 2-year-old, but far less so in that of a 44-year-old.
Pruning problem:
It remains to be seen whether the apparent drop in the numbers of amygdala neurons in adults with autism stems from neuronal death or a stalling of this maturation process, Schumann says. [However, adults with autism have fewer immature neurons than children with autism do, suggesting maturation is proceeding normally. This hints at the fact that the net decrease in amygdala neurons may be the result of neuron loss, Schumann says.]
Neurons in the amygdala of children with autism also have an excess of the mushroom-like protrusions that link up with other neurons. The density of these ‘dendritic spines’ also drops over time in individuals with autism. Typical individuals have fewer spines to start, but the number remains relatively stable throughout life, according to a second study described on Saturday3.
In that study, the researchers looked at postmortem brains from [16] typically developing individuals and [16] people with autism, ranging from [7] to 46 years old.
All brains start with more connections than they need. Over time, some of these are removed, or ‘pruned.’ The unusually large number in dendritic spines in children with autism may result from deficient pruning early in childhood. Alternatively, the typical pruning process may be overwhelmed by an unusually large number of neuronal connections in the amygdala, says Ruth Weir, a postdoctoral associate in Schumann’s lab, who presented the findings.
Either way, the results suggest that the amygdala of children with autism is hyperconnected, a finding in line with results from brain imaging studies. That two different methods have led to the same conclusion is striking, says Ruth Carper, assistant professor of neurosciences at San Diego State University, who was not involved in the study.
The two sets of findings might be related, Weir says. Hyperconnectivity at a young age could lead to increased stress on these neurons, which might result in cell death.
The researchers plan to investigate whether the brains that show an excess of neurons in the amygdala are the same as those with too many dendritic spines, says Schumann. She and her team also aim to determine whether the findings apply primarily to particular neuron types, such as those that excite brain activity or those that inhibit it.
For more reports from the 2016 Society for Neuroscience annual meeting, please click here.
References:
Recommended reading

Too much or too little brain synchrony may underlie autism subtypes

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Explore more from The Transmitter

Smell studies often use unnaturally high odor concentrations, analysis reveals

‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt
