A new look at walking in early childhood: Q&A with Rujuta Wilson
Quantifying toddlers’ gaits promises to improve autism diagnosis and intervention.

A baby’s first steps are a major developmental milestone—one that is often delayed in autistic children, many studies show. But the truth may be more nuanced, says Rujuta Wilson, assistant professor of pediatric neurology and child psychiatry at the University of California, Los Angeles (UCLA).
She and her colleagues analyzed walking in 51 autistic children ages 12 to 36 months and found they took their first steps within the same age range as 45 neurotypical children matched in chronological and mental age. But the autistic toddlers walked at a significantly slower pace. And the slower the child’s movements, the lower their developmental scores in other motor skills, communication and adaptive function. The findings were published in Autism Research in January.
More can and should be done to assess gait quality and the links between walking and other aspects of development, Wilson says. “Walking isn’t just the main way we usually get around. It also plays a fundamental role in the development in other areas, such as social engagement with others.”
The Transmitter spoke with Wilson about the methods used to quantify gait in toddlers and how these new techniques might influence research.
The interview has been edited for length and clarity.
The Transmitter: How should research on autism and motor skills advance?
Rujuta Wilson: Despite the prevalence of impairments in motor ability in autistic children, we don’t really have great clinical language to describe what specific differences we see. We often use terms like “clumsy” or “uncoordinated” or “abnormal motor signs.” As a neurologist, I think defining these differences would really help in understanding why they are occurring, and maybe in intervening clinically.

TT: What would you like to change?
RW: A lot of measures we use to probe motor ability take some level of cognitive ability to complete—for instance, not just the ability to grab coins, but to also insert six coins into a bin. The focus of my lab is to look at pure motor movements. The aim is to be more objective and quantitative in measuring motor skills and their quality in people with neurodevelopmental conditions, specifically autism. We’re interested in seeing what motor differences—particularly ones that aren’t contingent on other developmental domains, such as cognitive ability—may be specific to each condition.
TT: How do current methods fail children with neurodevelopmental conditions?
RW: When I was a fellow [at UCLA], we used a widely used standardized motor assessment to assess children with genetic syndromes and with autism. What we found was that almost all of the children hit the floor score: zero percentile. We weren’t able to measure any variability—nor disentangle whether this performance was due to fundamental motor deficits or cognitive ability, a lack of understanding. When we qualitatively looked at our data, we were able to pull out that they could not fundamentally anticipate, say, catching a ball, even after practice. It was a visuomotor coordination issue. It was something we worked on capturing more objectively.
TT: What kind of movements are you looking at now? What tools are you using?
RW: When it comes to what is known as duplication 15q syndrome, we’ve used tools such as pressure-sensitive gait mats. We’ve found children with this condition showed slower velocities, poorer postural control and more variability in their gait than both neurotypical children and age-matched children with autism without a genetic syndrome.
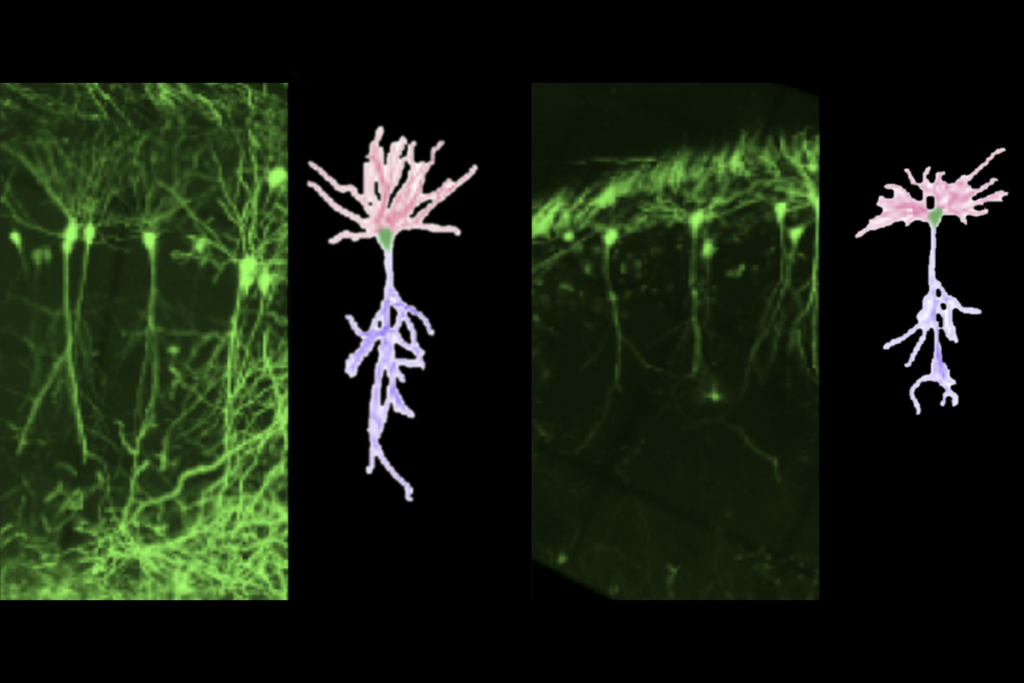
In some of our previous work, we’ve also placed wearable sensors and gyroscopes on the upper and lower bodies of infants across the first year of life. We found those infants who ultimately went on to have an autism diagnosis showed a repertoire of motions that were less variable and less complex.

TT: In your most recent study, you found that autistic toddlers started walking at the same ages as neurotypical children but moved at a slower pace. What might that mean?
RW: Often in pediatrics, the focus is on attaining developmental milestones. This means that during a well-child visit, if an autistic child starts walking when expected, fundamental differences in their gait compared with that of their peers may not be recognized.
If these differences are not recognized and intervened on, that could have other impacts on these children. They might not keep up with their peers—for instance, their slower pace may mean they may not have as much time with exploration on a playground—or impact their ability or motivation to play in activities.

TT: What do you hope to accomplish with the measures you are developing?
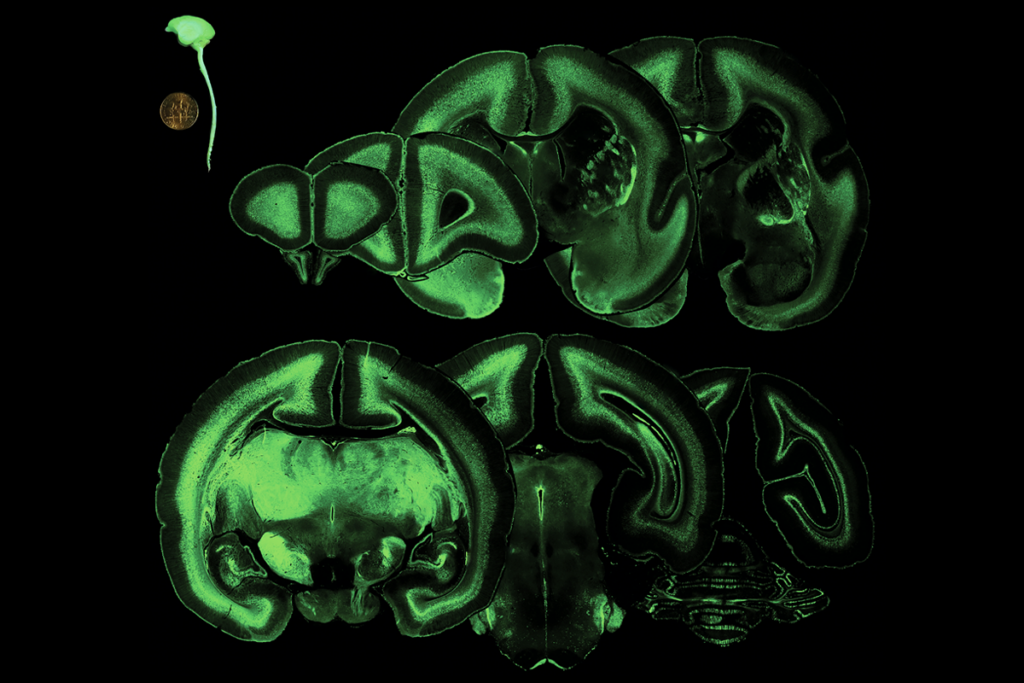
RW: Understanding how these differences in motor skills might appear as early as the first year of life could give us a way to diagnose autism at an earlier age. It can also inform interventions for these children, such as giving them more time to explore their environments to help enrich their development. And the more we can correlate these differences in motor function with things like electroencephalography or brain imaging, the more we might understand why they occur.
TT: What are your next steps?
RW: We’re moving in the direction of diagnostic instruments others can use to measure these motor differences we’re seeing. We’re thinking about and testing different ideas, and then we can start validating our findings and how we can make everything more scalable and clinically accessible.
We’d like to know the minimum duration of time an infant might wear sensors to detect these motor differences. If a clinical visit lasts from 15 to 45 minutes, can we collect the data we’d need in 10 to 15 minutes?
We’re also working on markerless tracking. Our gold-standard measure of gait uses wearable sensors and gait mats. We want to see if we can derive the same measurements of gross motor ability using just a video of a child. If the videos are captured correctly at home or in the clinic, we could use an algorithm analyzing that video to look for differences in motor quality that might relate to developmental concerns.

Recommended reading
Prenatal viral injections prime primate brain for study

Common and rare variants shape distinct genetic architecture of autism in African Americans
Explore more from The Transmitter

Executive function; screen time; Rett syndrome therapy
Emotional dysregulation; NMDA receptor variation; frank autism