‘Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s,’ an excerpt
In his new book, published today, investigative journalist Charles Piller tells the story of the scientific misconduct that shook Alzheimer’s disease research to its core, and the neuroscientist who helped to expose it.
To no surprise, Matthew Schrag spent the day before our first meeting in the lab. He’d been running computer-imaging experiments to refine his work on the Cassava dossier after an extended examination of other studies on PubPeer, a website where technical gumshoes post deconstructed Western blots, displaying telltale clip marks, halos, and shadows—signs that suggest copy-paste misconduct, such as the removal of a band from an image before publication, or insertion of another where it doesn’t belong.
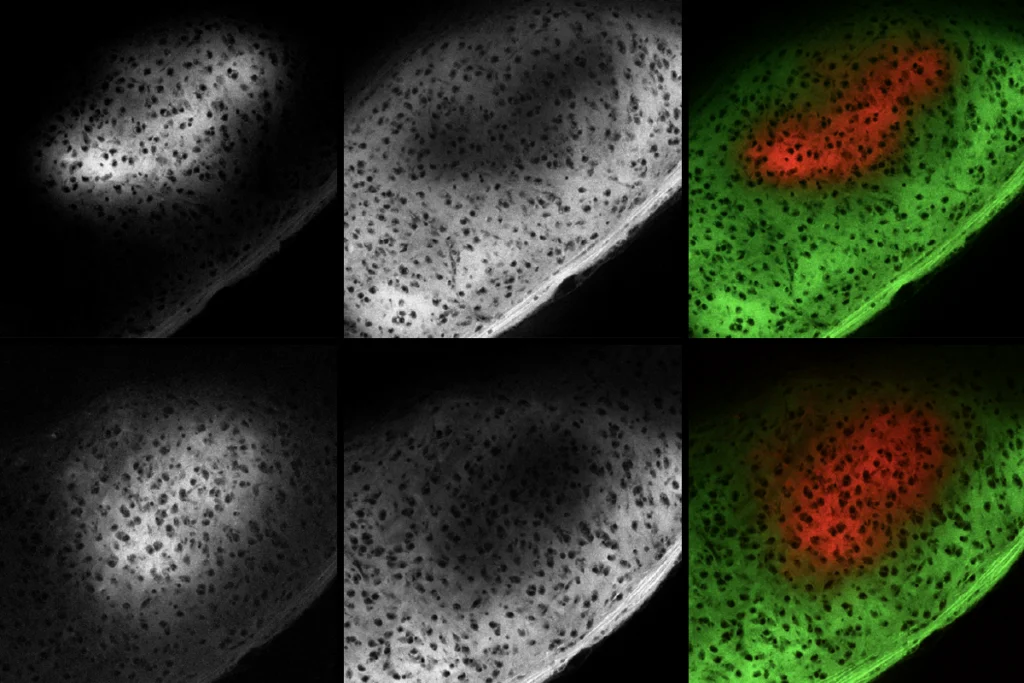
Schrag was looking to pull random examples of doctored blots in Alzheimer’s research to test out a new detection technique he was tinkering with. He wanted to quantify just how similar the suspect blots he’d collected for his Cassava dossier were to one another. Wary of injecting “expectation bias” into the test, he’d sought out random examples first rather than try out his method of identification on images that he already thought were probably improper. The first article on the results list, recently flagged by a pseudonymous critic, had appeared in the Journal of Neuroscience. The lead scientists on the paper were French researchers whose names were unfamiliar to Schrag. The experiment examined chemical transmissions in postmortem brain tissue to understand how acute brain injuries might be a risk factor for Alzheimer’s disease. The topic was of growing interest in the field, and the findings provocative—a link to how brain trauma might promote amyloid-beta production. It raised his eyebrows for another reason. One of the co-authors, Charles Glabe, was a noted Alzheimer’s researcher from the University of California at Irvine. His role had been relatively minor from what could be gleaned from the publication, but his name lent credibility. Sets of bands in two separate Western blots presented in the paper looked strikingly similar, if not identical, yet were said to represent different experimental conditions. The likelihood of such twinned bands is remote. The images offered an ideal test case for his new technique.
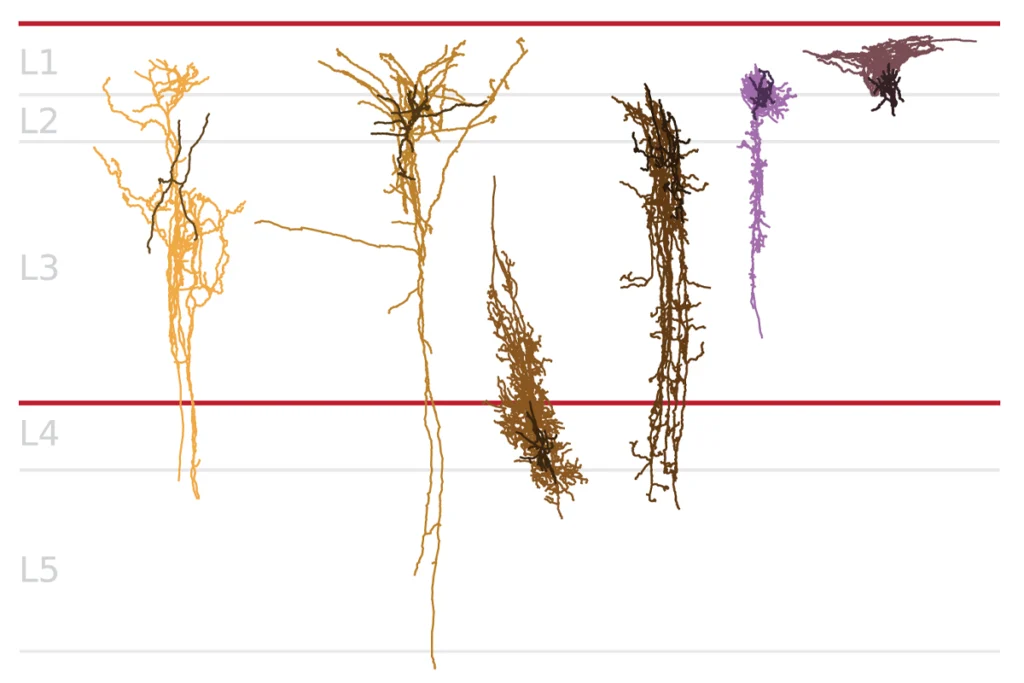
The dark bands on white backgrounds looked like silhouettes of flat-bottom smiles. First Schrag matched the two sets for size and contrast, ensuring an apples-to-apples comparison. To compare every detail, he colored one a brilliant fluorescent red, and the other green. Using NIH-approved software, Schrag merged the colored bands, displaying precisely overlapping areas in bright yellow. Areas that didn’t overlap would retain their red or green hue. To the naked eye, the merged bands looked 100 percent yellow. An identical match. Then to quantify his findings, Schrag calculated a correlation coefficient by tracking the similarity of every pixel—each tiny dot of the image. With thousands of such comparisons, he could calculate the strength of the overall relationship between the merged bands. Identical images—pixel-perfect—would show a correlation of 1.0. For genuinely different bands, a correlation above 0.7 or so would be rare. In this case, the bands showed a 0.98 correlation. Schrag’s years of experience and the logic of the science told him that identical- twin bands virtually never occur by chance. In his typically understated way, he called the correlation “remarkably high.”
That was December 21, one day before we first spoke. Schrag didn’t mention the test during our conversation. We were just getting started, after all. He wasn’t ready to share the first hints of the scandal of a lifetime.
As Schrag pored through the PubPeer list, he noticed that some of the same authors came up a few times. He tugged on that string, searching for the first and last authors on a couple of the papers. The first author usually does most of the writing, while the senior scientist—often a mentor or principal investigator for the experiment—normally takes the last slot. A throughline—the single name that appeared on every paper—floated to the surface. Schrag hadn’t heard of him among the multitudes of Alzheimer’s researchers. But then he noticed that the scientist was lead author on one of the most cited papers in many years. This was an ascending neuroscience talent: Sylvain Lesné at the University of Minnesota.
Cheaters cheat, right?
During the five months he had spent refining his Cassava dossiers, Schrag’s thoughts returned over and over to a central worry that he gradually realized he’d need to face: Could this be more than a single set of bad papers, a lone bad actor, or a wayward lab? Could there be many more lapses and fakes in Alzheimer’s research that few in the field wanted to acknowledge, let alone confront? If so, important research might be based on wobbly foundations. Just as bad, research might be detoured into costly dead ends. “Everybody thinks that scientific integrity issues are very, very rare. I can’t say I’ve ever been asked to review a paper where I went into it saying, ‘I don’t trust these guys. They’re gonna cheat on me,’” Schrag said, conceding that the apparent misconduct had left him unnerved. “I don’t think that’s how people think about scientists,” he added, sounding more hopeful than convinced. For the first time, Schrag found himself questioning a bedrock assumption about his chosen profession. He knew that the alternative—a breakdown of trust—could taint an entire research direction. Did the Lesné articles rise to that alarming level, possibly more alarming than Wang’s seemingly blatant doctoring? It was too soon to tell. The detection of phony images is part art, part science, and not always clear-cut. But even when some doubtful Western blot or micrograph doesn’t quite meet the threshold that demands public exposure, prudent scientists would steer around dubious work to avoid investing efforts in the wrong places. If they knew about it.
“Knowing where the land mines are can keep you out of trouble,” Schrag said. He couldn’t stop thinking that Alzheimer’s research needed one of their own to turn the microscope around, to get a clear focus on what corrupt scientists might be up to. Bring it on, he thought. As he said to me during our very first conversation, he wanted to protect “my scientific space.”
It also became clear that, almost like an investigative reporter, Schrag seemed to find thrills in the hunt; a chance to right a disturbing wrong— even if the implications for the field disturbed him.
“Cheaters cheat, right?” he said during our next conversation. “So, when I pulled up Lesné’s name on PubPeer and three or four other papers came up, I started to wonder. If somebody might be cheating three or four times, there’s likely to be a ton of stuff here for me to work with.” As Schrag began to check other Lesné writings that hadn’t been flagged on PubPeer, land mines exploded everywhere. “Within a day or two, I found out that ton of questionable stuff [had appeared] in Brain and PNAS and Nature,” among the world’s leading journals.
Schrag had stumbled upon the seminal Nature paper in which Lesné and his mentor Karen Ashe, a top neuroscientist, unveiled their star protein, amyloid-beta star 56 (Aβ*56). Since it appeared in 2006, that study had been cited thousands of times by other scholars, some of them the top names in the field, including Harvard’s Dennis Selkoe, a chief progenitor of the amyloid hypothesis; his UK counterpart John Hardy; University College London luminary Bart de Strooper; and University of Zürich’s Adriano Aguzzi.
Lesné, first author of that study, Ashe, and their colleagues seemed to prove that when Aβ*56 was injected into rats it caused something like Alzheimer’s dementia. The study’s emergence came at a moment of discouragement—even despair—for the amyloid hypothesis and placed it back at the center of the patients’ and the pharmaceutical industry’s focus. The Nature paper offered strong support for a new organizing principle: If old, failed drugs targeted sticky amyloid-protein plaques, new ones should try to attack, as much as possible, the elusive oligomers floating in the cerebrospinal fluid—even if removing plaques remained a concurrent goal. Drug developers saw new opportunities, and federal funders soon lavished vast sums on oligomer research.
Lesné soared in the aftermath, becoming an assistant professor at UMN with his own NIH-funded lab in 2009. Aβ*56 remained a primary research focus. And in May 2022, Lesné received a coveted R01 grant from the agency, securing him up to five years of support. (The NIH program officer for the grant, Austin Yang, co-authored the 2006 Nature paper. When I reached out to Yang later, he declined to comment.)
If Schrag’s doubts were correct, Lesné’s findings were an elaborate mirage.
Schrag quickly identified twelve other papers that directly concerned or described Aβ*56 that appeared to have been doctored. Lesné’s fingerprints were all over them. Ashe had co-authored five. (He also found other deeply suspect Lesné papers, written without Ashe, on related or different issues.) Schrag had reached a crossroads. If he was right, he would have to cast serious doubt on a key advance in his field. Sham experimental results had been treated as established fact with enormous influence. If he exposed the case, Schrag realized, fresh doubts about the amyloid hypothesis would surely burst into view. His findings could set back—or even provide ammunition to derail—the dominant view of how to cure one of the most terrifying diseases of our time.
“It became clear to me very quickly that not only was this going to be a case for me to practice this technique on and make sure it was working,” Schrag told me months later. “I was going to have to tell the NIH that this was an issue. The journals were just too big. The papers, the concepts were too big.”
Excerpted from “Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s,” by Charles Piller. Reprinted with permission from One Signal Publishers, an imprint of Simon & Schuster, Inc. Copyright 2025.
Explore more from The Transmitter

A scientific fraud. An investigation. A lab in recovery.
Microglia’s pruning function called into question