Preprint questions validity of postmortem brain studies
But the alternatives, including living-brain biopsies, raise logistical and ethical questions, experts say.
Patterns of gene expression in the human prefrontal cortex vary depending on whether the tissue donor was living or deceased, according to a new preprint.
The magnitude of change for each gene is modest, but the effects are widespread, involving roughly 80 percent of genes.
The findings suggest postmortem brains are a poor stand-in for living brains in studies of neurological conditions, including autism, the researchers say, though several scientists disagree.
“The implications are real,” says study investigator Alexander Charney, neurosurgeon and associate professor of psychiatry, genetics and genomic sciences at the Icahn School of Medicine at Mount Sinai in New York City. “People are going to have to decide how these findings impact their work.”
Charney says he and his colleagues were about to launch a clinical trial of an Alzheimer’s disease drug, the target of which was identified in an analysis of postmortem brains. “As a result of these findings, we put the brakes on that,” he says.
But other researchers say there’s nothing surprising about gene expression variation between living and postmortem brains, and the divergence has no bearing on the usefulness of postmortem brain studies: What matters is the difference between brains with and without disease.
“I believe the conclusions they’ve drawn from the differences they see are very premature, and I think their claim that the postmortem brain does not reflect disease at the molecular level is unfounded,” says Daniel Weinberger, professor of psychiatry, neurology, neuroscience and genetic medicine at Johns Hopkins University School of Medicine and director of the Lieber Institute for Brain Development in Baltimore, Maryland.
“The paper has interesting data, but it’s not asking interesting questions and carefully considering what the data are showing,” says Bernie Devlin, professor of psychiatry at the University of Pittsburgh School of Medicine in Pennsylvania, who was not involved in the work. “The conclusions from the data are just plain off-track.”
C
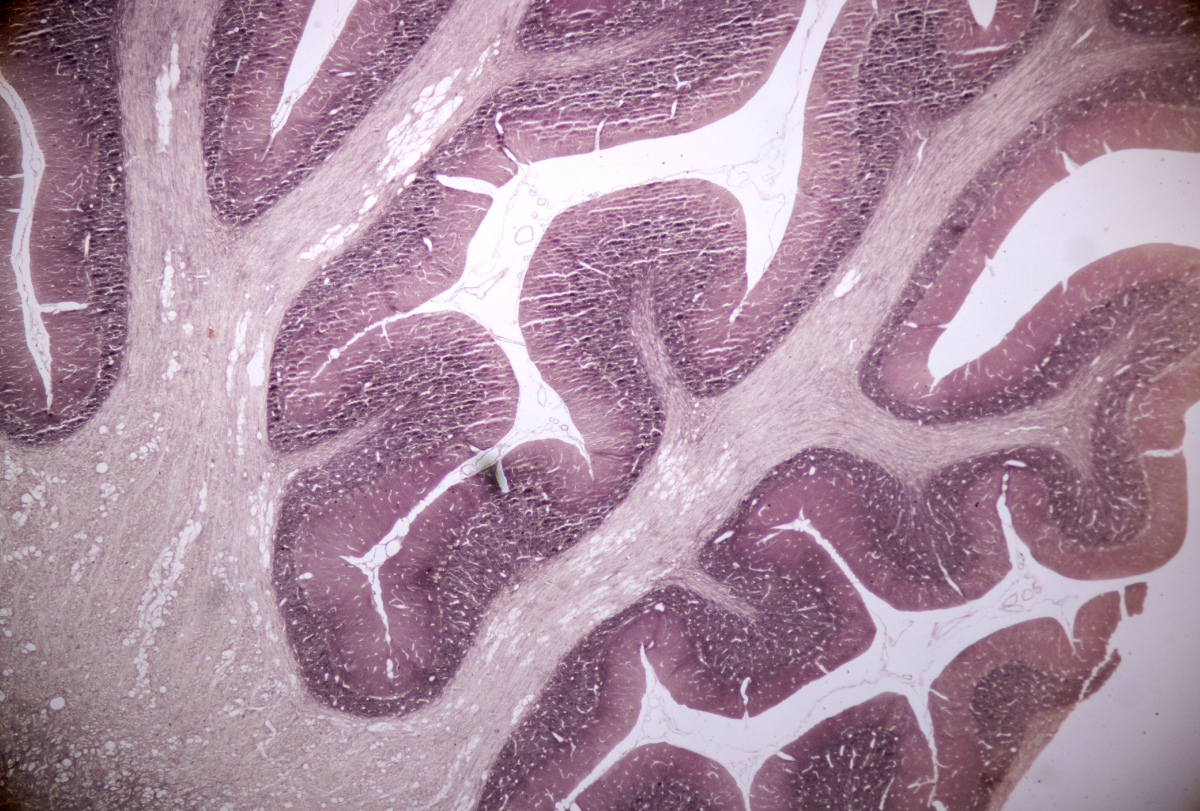
harney and his colleagues started their research 10 years ago to test the assumption that studies of postmortem brain tissue can reveal mechanisms of neurological disease, given the fact that RNAs degrade quickly after death. That’s why brain banks document the postmortem interval — the length of time between death and the preservation of brain tissue — and strive for the shortest interval possible.The team sequenced RNA in chunks of prefrontal cortex tissue from 246 deceased donors and 289 living donors, matching the two groups as much as possible based on age, sex and neurological diagnosis. Frozen postmortem tissue came from three brain banks in the United States, and the postmortem intervals ranged from 20 minutes to 38 hours.
The tissue from living donors was collected during surgery to insert electrodes for deep brain stimulation, an elective procedure for conditions such as Parkinson’s disease and obsessive-compulsive disorder. The procedure typically involves cauterizing a small amount of tissue to make room for the implant. The researchers modified the procedure to instead biopsy and immediately freeze the tissue, at no risk to the patient.
The two groups show statistically significant differences in gene expression across 17,186 genes, the team found. The magnitudes of the differences are on par with those observed in studies comparing gene expression in postmortem tissue from people without and without neurological conditions, Charney says.
“The effect is not huge, but almost every gene is affected,” he says. “The overall co-expression of genes is kind of rewired.”
Most of the tissue in the study came from people with Parkinson’s disease. But the differentially expressed genes the study uncovered overlap with those previously found to be altered in postmortem tissue from people with autism, Alzheimer’s disease or other neurological conditions. The team posted their findings to the preprint server medRxiv in April.
“In the postmortem state, when you compare cases and controls, you’re seeing some interaction between the disease process and the death process,” Charney says. “Our brains are way more similar to each other than they are to any dead brain. The living-brain-dead-brain difference kind of dwarfs any disease difference.”
I
n addition to the largely critical reactions to the preprint’s conclusions, some experts also took issue with the actual data. Weinberger says the researchers did not adequately control for RNA degradation in either type of tissue, and the integrity of RNA in tissue from living donors was lower, on average, than that in postmortem tissue — a finding he calls “surprising.” Living tissue samples also had a smaller proportion of neurons than postmortem samples.“They’re treating the living samples in this study as if they’re the gold standard, but there’s a lot of tarnish on this gold,” Weinberger says.
All model systems have pros and cons: Brain organoids are stuck in a fetal state; mice are not people; and postmortem brains are not living brains. Even living tissue has the limitation of reflecting the consequence of disease rather than the cause, says Stephan Sanders, professor of neurogenetics at the University of Oxford in the United Kingdom, who was not involved in the study. “This paper, I think, falsely makes too much of a problem and doesn’t offer solutions.”
The paper does propose one solution, though: to use living-brain biopsies instead of postmortem tissue. But reactions to this idea were particularly sharp.
“The idea that you’re going to replace postmortem studies because you can biopsy 1 centimeter of prefrontal cortex in the living brain, I think, is a bit over the top,” Weinberger says.
“Just because you can do this in Parkinson’s disease doesn’t mean it’s possible in autism, schizophrenia and Alzheimer’s. No one is going to consent to that,” Sanders says. “So why say we should no longer do postmortem studies? A much more helpful statement is: ‘We need to embrace all models, and living brain tissue could help us with our interpretation.’”
Sanders says researchers should use the new data to control for changes in gene expression associated with the death process. That’s possible in theory, Charney says, but more work is needed. “A lot more groups need to be asking the same question about what postmortem tissue can and can’t be used for.”
Charney says he and his team have done single-cell RNA sequencing from living and deceased brain donors and found the same pattern of differential gene expression across neurons and non-neuronal cells, such as astrocytes, microglia and oligodendrocytes. The pattern persists in a comparison of protein expression between the two tissue types, too, Charney says.
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
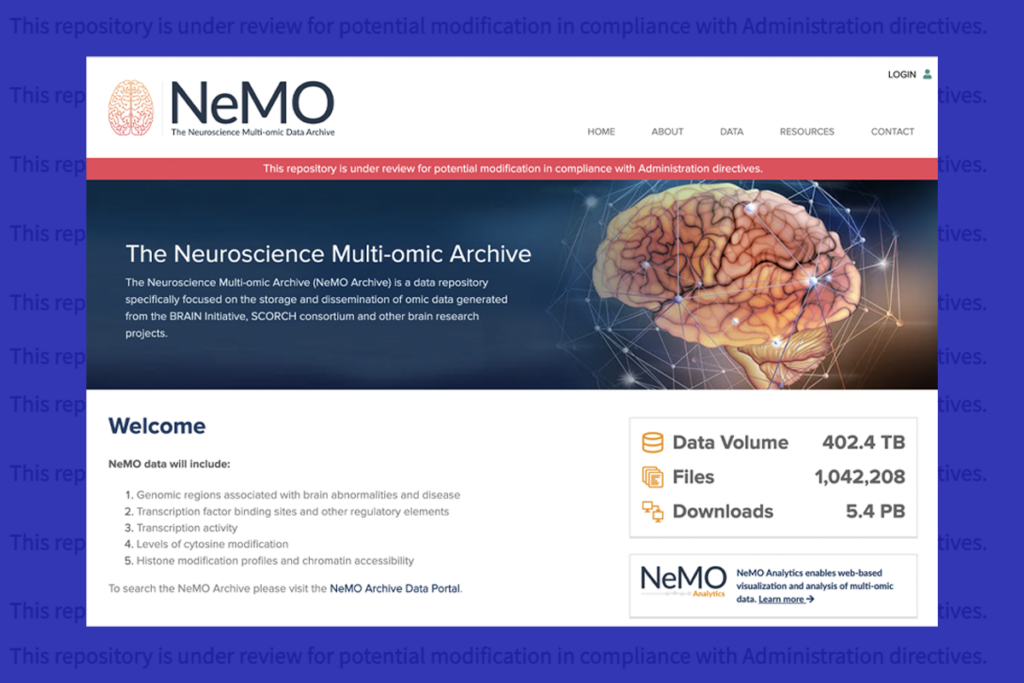
U.S. human data repositories ‘under review’ for gender identity descriptors
Explore more from The Transmitter

‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt

