In late January, a new pain medication was the first non-opioid to gain U.S. Food and Drug Administration (FDA) approval in more than 20 years. The drug, suzetrigine (marketed as Journavx), works by selectively blocking a sodium channel. Its approval represents a milestone for basic pain researchers who have been trying to unravel the mechanisms of these channels for decades.
Research first implicated NaV1.8, suzetrigine’s target, in pain processing in 2002 and another sodium channel, NaV1.7, in 2004. Inflammation or nerve damage can lead to overexpression of these channels, which causes pain-sensing neurons to fire excessively and results in chronic pain. Despite a host of preclinical work, no treatments are approved to specifically target NaV1.7.
“A gold-standard pain molecular target still doesn’t have a drug that targets it after all of these years. And then what does that say for all the other potential targets?” says Mark Zylka, professor of cell biology and physiology at the University of North Carolina at Chapel Hill.
One potential reason for that lack is that basic pain research is often not clinically relevant, according to a review of NaV1.7 preclinical studies published in October in PAIN.
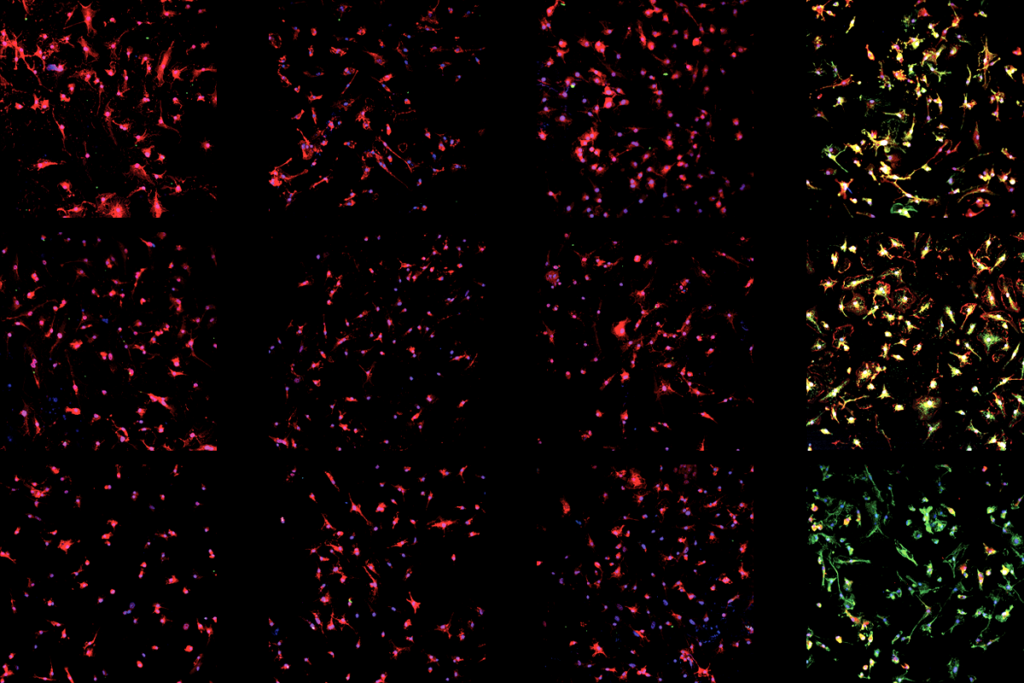
Few of the 44 preclinical studies testing drugs that block NaV1.7 used repeated doses, according to the review, even though tolerance can develop after the first dose, and other sodium channels can compensate for its lack of function, a phenomenon called degeneracy. The studies also lacked genetically diverse animal models, used primarily male animals and relied on nonstandardized pain behavioral models and measurement scales—making basic findings difficult to translate to human treatments.
Despite the FDA’s approval of suzetrigine, there needs to be continued research of the drug’s long-term efficacy, says Steven Prescott, professor of physiology at the University of Toronto. “Maybe there’s still risk of compensation, but, you know, maybe they were lucky. We haven’t actually seen the chronic data yet.”
Prescott and his review co-investigator Stéphanie Ratté, senior research associate in Prescott’s lab, spoke with The Transmitter about how they selected studies for the review, as well as what their findings mean for basic neuroscientists who study pain.
This interview has been edited for length and clarity.
The Transmitter: How did you select preclinical studies for your review?
Steven Prescott: What we mean by preclinical in this context is all animal research, specifically focusing on rodent models of pain. There isn’t any formal distinction between fundamental basic discovery science and precursors to clinical trials. We didn’t want our review to be critical of what people have done because in many cases, their research wasn’t intended as a precursor to clinical studies.
Stéphanie Ratté: We looked at everything that used NaV1.7 inhibitors, because the distinction between preclinical and basic research is not so clear. People will make assessments about how a drug works in some studies that are not designed as a precursor to clinical trials. A lot of these papers are looking at mechanisms of pain, but they applied a specific blocker and looked at the resulting behavioral outcome. Does it stop, reduce or do nothing for pain?
TT: What needs to change in the basic pain neuroscience field?
SP: Different people probably have their own favorite answer, like we should use more human tissue, animal behavioral testing needs to change, or we need to improve the reproducibility of tests. These answers are all probably correct, but the question is how do you do all of this? We shouldn’t neglect one thing in favor of another. How do we take the strengths of different models and cobble them together?
SR: It’s not working. Everybody will disagree about what we need to change, but something that everyone might agree on is having a set of registered preclinical studies that are designed more similarly to clinical trials where it is blinded, randomized and in a larger number of animals. That would take us closer to a successful transition from basic research to clinical trials. But there needs to be money available for this.
TT: Do basic pain researchers need to be thinking about the clinical applications of their work?
SP: I would say yes because it’s motivating, and if you’re not thinking about translation, then you’re missing opportunities. At the same time, I don’t think there should be a preoccupation with this. I think basic pain researchers are a little too quick to focus on “what’s the cure for pain?” and the clinical translation. Because of that, maybe there’s been less focus on fundamental mechanisms like homeostatic degeneracy.
Eve Marder, for example, has been a huge proponent of degeneracy, looking at it in lobsters. There are other people picking up these concepts for things like epilepsy, a field that has suffered from very similar problems in developing effective drugs. If these concepts had permeated the pain field earlier, it might have been helpful for thinking about how the nervous system responds to treatment. I don’t know a lot of basic pain research thinking about the learning and memory aspect of the pain system.
SR: There’s a very pressing reason to do this work. I have to say it is sometimes difficult to have the patience to try to study the basic mechanisms when there is a very pressing problem with chronic and neuropathic pain. There are so many papers where one thing is manipulated, and then the conclusion is “now we can cure pain.” I think when basic researchers find something that seems to change the behavior of the animal, instead of publishing it as a cure for pain, the next question would be asking if there is a reason this wouldn’t work in humans. If we explore this, that would make the results so much more robust. A little bit of skepticism would be good.
TT: What can researchers do to address the issues highlighted in your review, such as genetic diversity in animal models, standardizing behavioral models and finding objective markers for measuring pain?
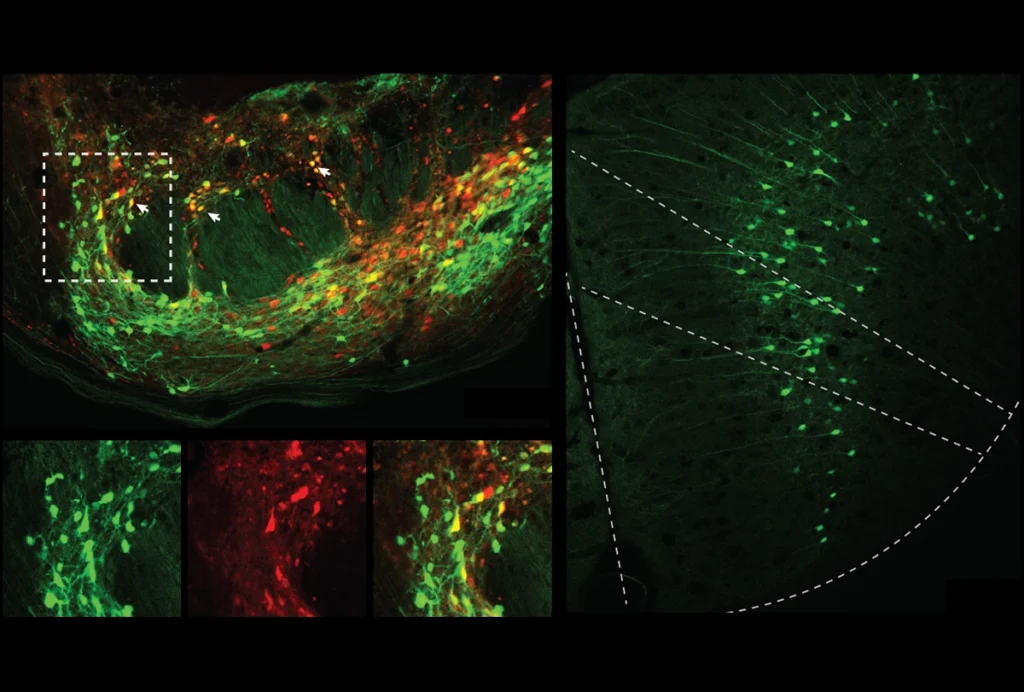
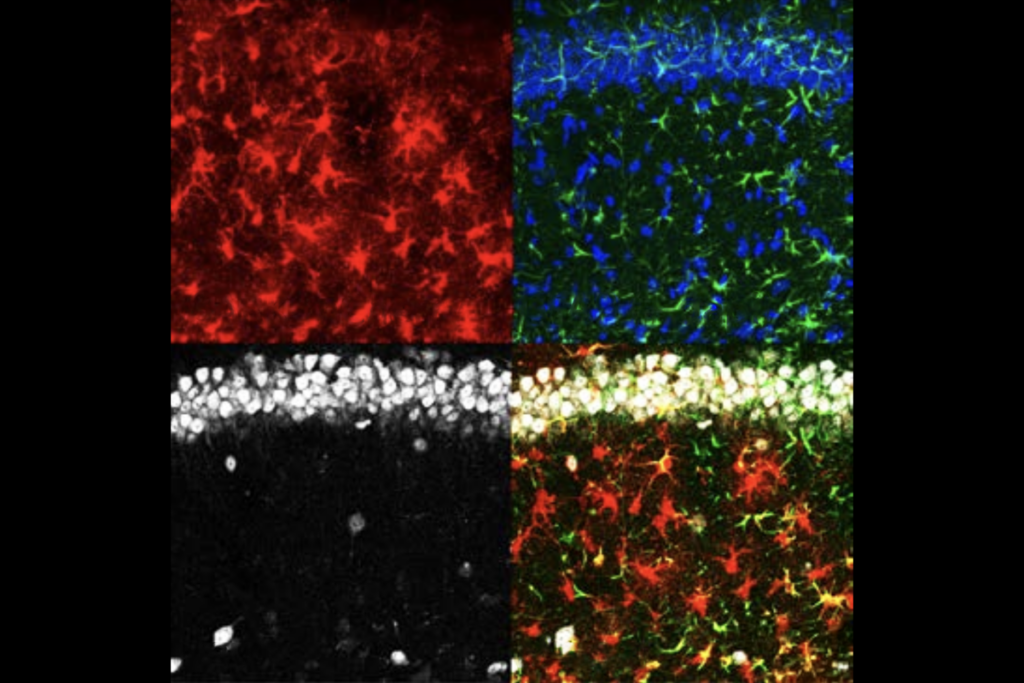
SP: You can test multiple strains or outbred strains that do have more heterogeneity, and that includes testing a broader range of animals, including older animals as opposed to just targeting young animals. But one important consideration is there’s limited time and limited money to do these tests, so how can you do it reasonably fast and reasonably objectively? Some labs have developed robotic testing, which has higher throughput and is more objective. RAMalgo is the name of our lab’s robot. We wanted to make things more reproducible and more objective when trying to do conventional pain reflex-based tests. Spontaneous pain can be very subjective, but there are machine-learning tools that can help. Mark Zylka with the software platform PainFace, for instance, has tried to push in the direction of being more objective and efficient in scoring things other than reflexes.
SR: We cannot ask animals if a stimulus is painful or not, but that’s the easiest way to determine pain in humans. There’s a lot of possibilities with machine learning and artificial intelligence to measure ongoing pain or non-reflexive behavior. AI can maybe detect things that we would not be looking for and spot things that are quite subtle. Developing these methods using robotics and machine learning are part of our greatest effort in our lab right now.