Psychiatric conditions have long been regarded as issues of “mental health,” a term that inherently ties our understanding of these disorders to the brain. But the brain does not exist in a vacuum. Growing evidence over the past 10 years highlights a link between the body and what we think of as mental health. Many studies, for example, report that the peripheral immune system is altered in people who experience neurological and psychiatric conditions, including mood disorders, anxiety and schizophrenia.
Researchers traditionally assumed that peripheral inflammation was a downstream effect of these conditions, but basic research is now revealing that the immune system, the gut microbiome and peripheral inflammation are not just bystanders or results of psychiatric conditions—they are active participants and may hold the key to new treatments. Scientists are beginning to uncover the mechanisms by which the body influences the brain, challenging the notion that mental health is solely a matter of brain chemistry and reshaping ideas on the etiology of psychiatric disorders.
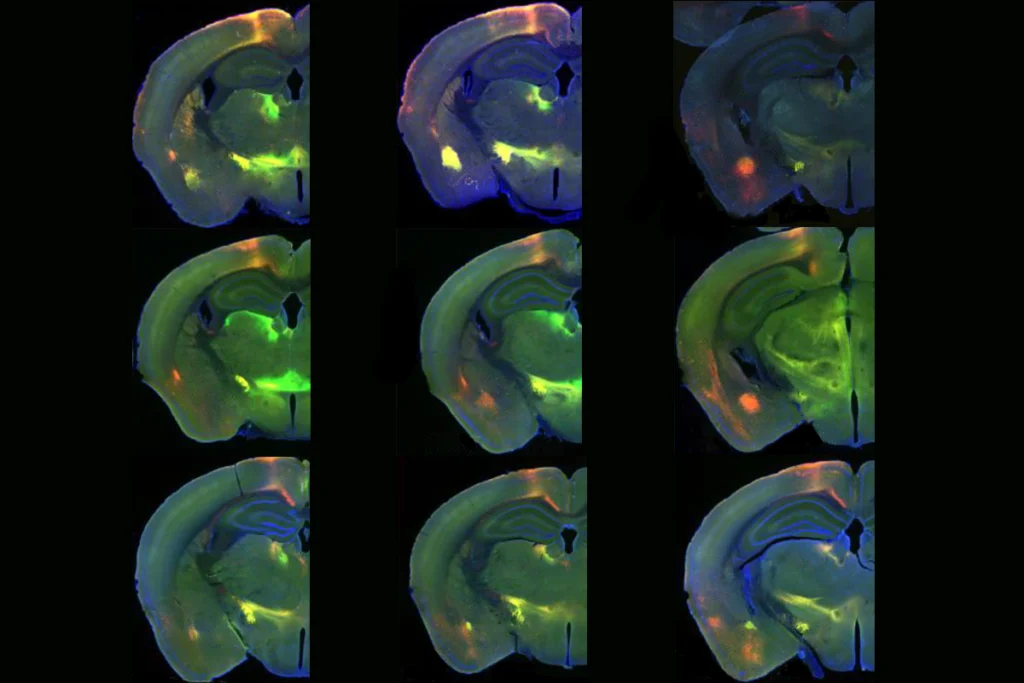
Like other neuroscience groups, we started our work in this area with the “brain-first” perspective: the idea that immune changes in the brain trigger stress-induced changes in behavior and peripheral inflammation. Our earliest studies supported this idea, demonstrating that directly infusing an inflammatory molecule, the cytokine interleukin 6 (IL6), into an area of the brain associated with reward behavior made male mice more likely to avoid others.
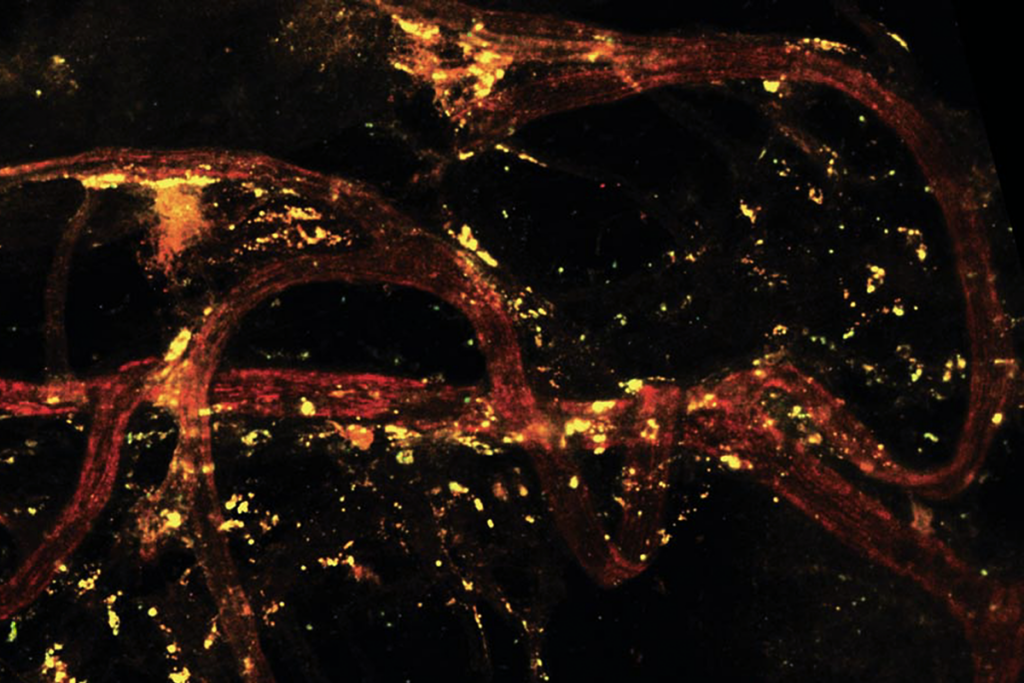
Our later work, however, found that the source of IL6 in the brain is actually peripheral immune cells. Either stopping the immune cells from producing this molecule or just blocking it from entering the brain made the animals resilient to social stress. These studies offered some of the first evidence that treating the body with a compound that does not cross the blood brain-barrier could prevent a brain-mediated behavior. Before this, blood markers were considered only indirect indicators of brain changes—and not direct mediators or potential targets for treatment.
T
he concept that the body is the root of emotions is not new. In the mid 1800s, Williams James and Carl Lange proposed that emotions result from the brain’s interpretion of the physiological response of the body—in other words, first you run away; then you are afraid. In the 1920s, James’ student Walter Cannon adapted this idea into a model in which brain processing promotes both concious awareness of a threat and a physiogical response. In the early 20th century, an emphasis on the role of the conscious brain diminished interest in the impact of physiological signaling on emotion. But groundbreaking neuroscience by Joe LeDoux’s group in the late 20th century renewed some notice of the Cannon-Bard (Philip Bard was a student of Cannon’s) and James-Lange theories by delinating the timing of neural signaling pathways of peripheral sensory information to the brain that produce emotional responses and shape learning.Meanwhile, as neuroscientists focused on conciousness, endocrinologist Hans Selye popularized the term “stress” to mean an endocrine adaptation to emotional and physical threat. As Selye initially proposed in the 1930s, many of these adaptations actually involved the peripheral immune response. When neuroscience, endocrinology and immunology started to merge into the field of neuroimmunology at the beginning of the 21st century, a concept similar to the James-Lange theory evolved from immune research on sickness behavior; specifically, the emotional experience of “stress,” and possibly depression in some people, was their brain’s interpretation of an immune response in the absence of a known physiological cause. For example, in rodents, injecting lipopolysaccharide—a component of gram-negative bacteria—into the body has lasting effects on cytokines in the brain, along with social and hedonic behavior, beyond the initial peripheral inflammatory immune response, similar to the effects of an exposure to a stressor.
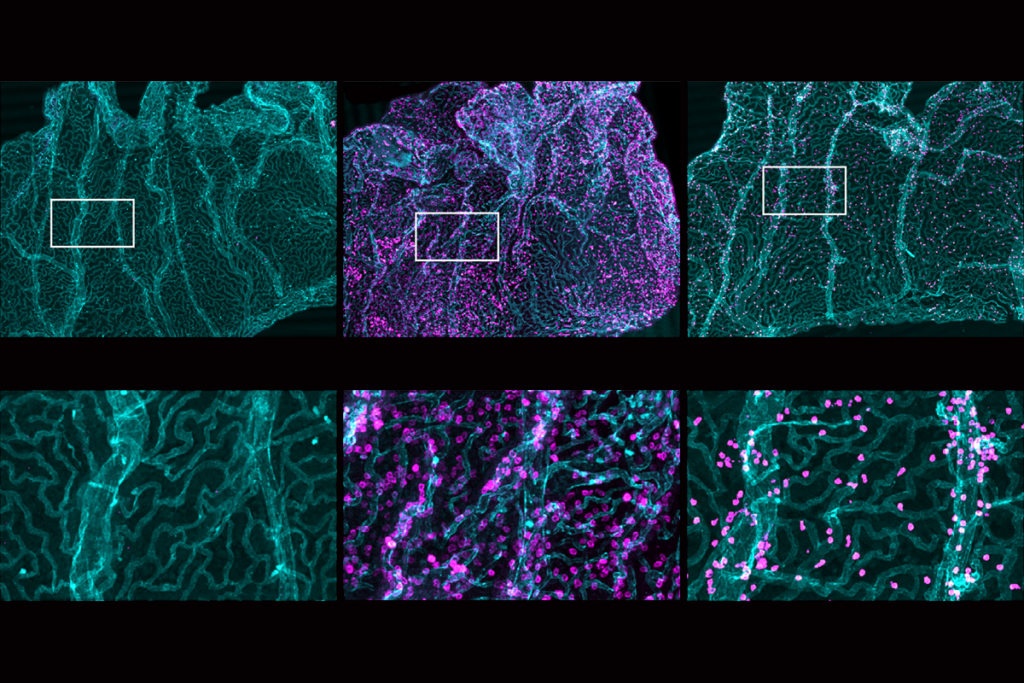
Research in the past decade supports the idea that stress itself activates the peripheral immune system, inducing an upregulation of many cellular and protein signaling components of the innate immune system in the body. Studies suggest that signaling proteins such as cytokines, or potentially even peripheral immune cells themselves, infiltrate the brain during and after stress exposure. Other work suggests that the gut microbiome contributes to anxiety-associated behavior in rodents, indicating that peripheral inflammation could be part of an endocrine messenger system that contributes to the gut-brain axis.
A paper published last year highlights peripheral factors’ role in human brain health. Researchers reported that a matrix metalloproteinase (MMP8) released from immune cells crosses into the brain, modifying reward circuitry in stressed mice and in people with depression. MMP8 may provide one of the first genuine biomarkers for depression and a new potential peripheral target to treat mood disorders.
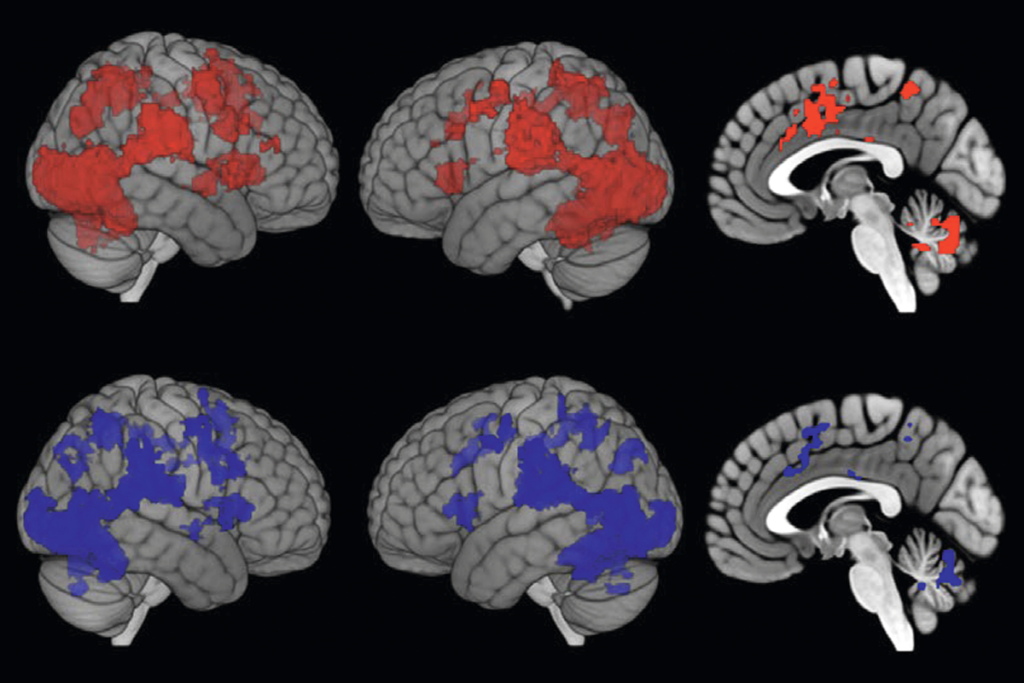
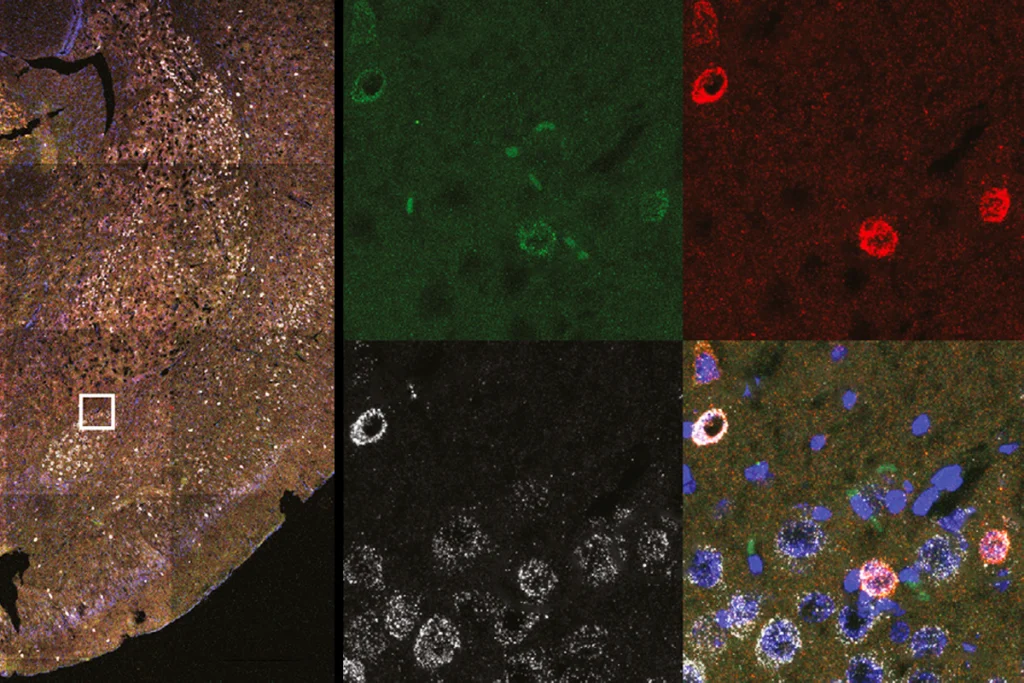
Additionally, recent research indicates that stressful experiences increase blood-brain barrier permeability, potentially making it easier for immune signals to infiltrate the brain. We have long known that certain diseases, such as multiple sclerosis and stroke, enable peripheral cells and their signaling molecules to invade the parenchyma. But growing evidence suggests that some immune cells get into the brain even in healthy animals. Stress can alter tight junction proteins in specific brain regions, making some areas more permeable than others and thus more susceptible. Individual and sex differences in the permeability of some regions under typical and stressed conditions may help account for differences in the prevalence of mood related and substance-use disorders.
As a field, we are still trying to understand the temporal and causal relationships between inflammation in the gut, body and brain. Advancing our search for effective treatments beyond the brain will revolutionize how we alleviate emotional and cognitive symptoms across disorders. It opens the door for new interventions that can fill treatment gaps or augment existing therapies. In animals, a treatment derived from the microbiome’s metabolism of polyphenols promotes resilience to stress by both reducing inflammation in the periphery and altering plasticity in the brain. In people, a mental and physical (MAP) training technique that targets the body and the brain by combining mindfulness practices with aerobic exercise reduces scores on depression indexes and rumination.
The future of psychiatric treatments lies in embracing the complexity of the mind-body connection. By expanding our focus beyond just the brain, we can develop effective therapies that address the root causes of mental health disorders. This approach also underscores the importance of interdisciplinary collaboration, integrating insights from neuroscience, immunology, gastroenterology and even osteopathic medicine to revolutionize how we understand and treat psychiatric conditions. As our understanding of the body’s influence on the brain continues to grow, so too will our ability to provide more comprehensive care for those struggling with mental health issues.