Unlike traditional antidepressants, ketamine acts quickly to relieve depression symptoms, and its effects last long after the drug has cleared the system.
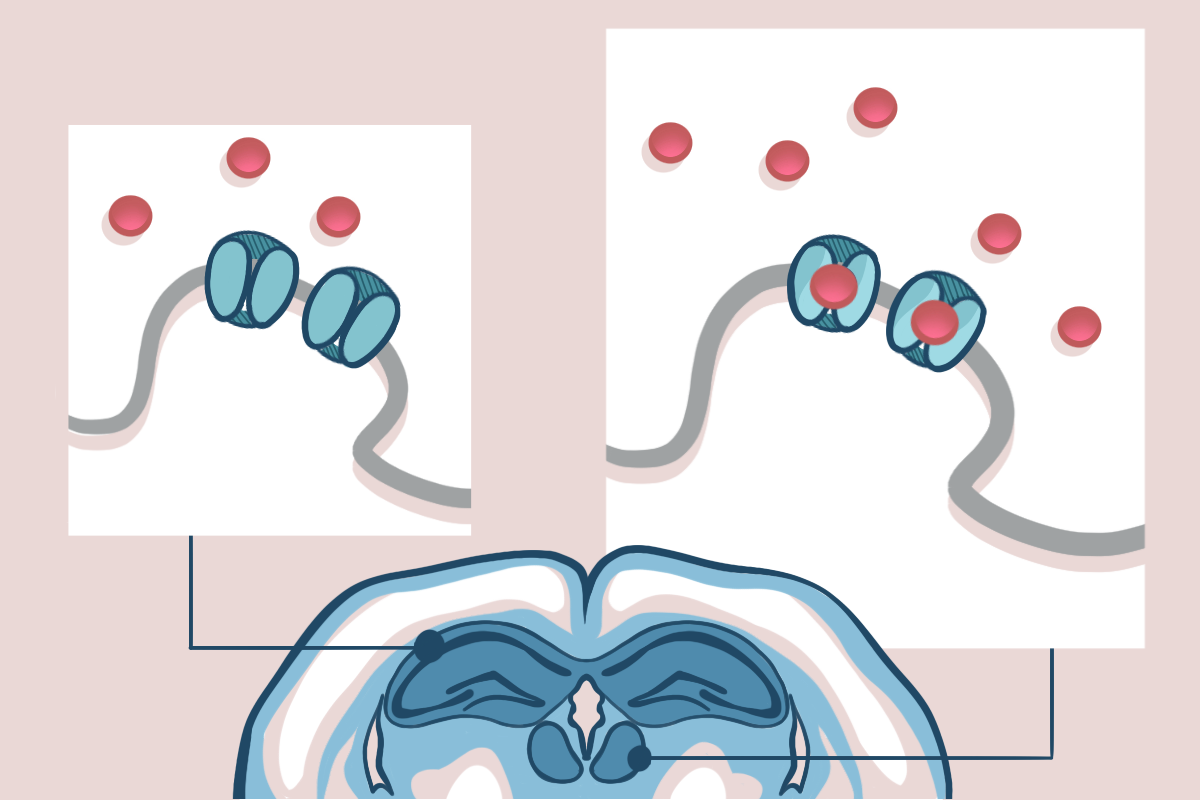
Researchers have puzzled over what ketamine is doing in the brain to achieve these results. For one thing, the drug acts on N-methyl-D-aspartate (NMDA) glutamate receptors, which appear on neurons all over the brain. “Then the question is: Does the drug hit on all these brain regions simultaneously?” says Hailan Hu, professor of brain science at Zhejiang University. Or does it affect one region first, which sets off a series of downstream antidepressant effects?
The answer is the latter, Hu and her colleagues report in a new study. Ketamine acts first on neurons in the lateral habenula, they found, in mice with depression-like symptoms. The structure—known as the “anti-reward” center—is hyperactive in people with depression and in mice modeling the condition, previous work has shown. That activity makes it highly susceptible to the drug’s effects, Hu and her colleagues discovered. Ketamine binds the NMDA receptors of cells in the lateral habenula and renders them inactive, which in turn interrupts downstream mechanisms of depression.
The findings, published in Science in August, help explain how the known targets of ketamine are involved in such a rapid antidepressant response, explains Christophe Proulx, associate professor of psychiatry and neuroscience at Laval University. Proulx was not involved in the work but co-authored a Perspective article on it.
Spotlighting the lateral habenula’s role also represents a new way of thinking about ketamine’s effects on depression—involving a shift away from a focus on weakened circuits and impaired plasticity, says Todd Gould, professor of psychiatry and neurobiology at the University of Maryland School of Medicine, who was not affiliated with the study. “[The work provides] additional strong evidence supporting a different view about how ketamine may be working.”
A
lthough ketamine inactivated NMDA receptors in the lateral habenula of the depressive-like mice, it had less impact in the CA1 region of the hippocampus, Hu and her colleagues observed using in-vitro slice electrophysiology and electrode recordings in awake animals.When the researchers exposed the mice to a foot shock, which activated the animals’ hippocampal cells and opened the local NMDA receptors, ketamine then blocked the receptors in that region. Conversely, inhibiting activity of the lateral habenula neurons by way of optogenetics prevented ketamine from blocking the receptors, the team found.
Because the lateral habenula is so active in people with depression and in animals modeling the condition—it exhibits patterns of bursting activity—ketamine can have its inhibitory effect almost as soon as it reaches the area, which helps explain why the drug is so fast-acting, Proulx says. “The fastest way to have the effect of ketamine is by directly blocking an NMDA [receptor] on hyperactive neurons that induce depressive-like symptoms.”
These new findings also point to why ketamine has such a long-lasting effect, Hu says. The drug specifically acts on the brain’s open NMDA receptors by blocking their pore region and preventing ions from flowing through. Once the drug is in the channel, it has a slow rate of removal, Hu explains. And the lateral habenula in particular does not have a large store of NMDA receptors to replace blocked receptors, further prolonging the inhibition.
T
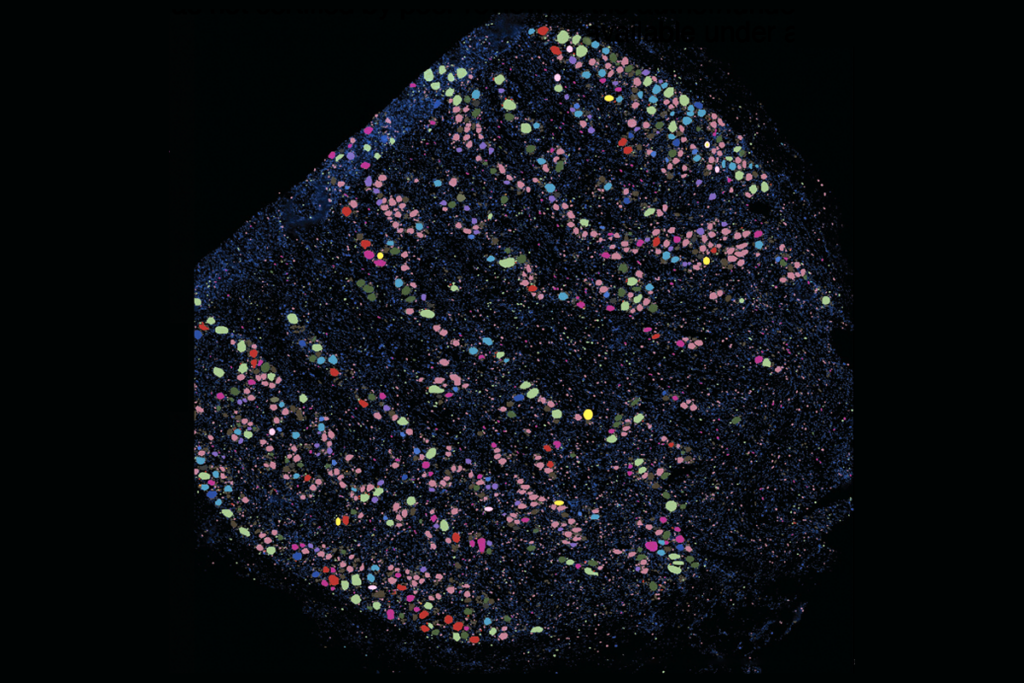
he lateral habenula regulates both the dopaminergic system and the serotonergic system. As a result, quieting the lateral habenula’s hyperactivity during depression has significant downstream effects, Hu and her colleagues found.The team engineered mice to lack the gene NR1—which encodes NMDA receptors—in the lateral habenula only. Doing so again disrupted the region’s bursting activity and mimicked the effect of ketamine.
Normally, levels of the neurotrophic factor BDNF increase in the hippocampal area after ketamine treatment. But removing the NMDA receptors blocked this increase in the mice, suggesting that the effect depends first on signaling in the habenula, Hu says.
Those findings help reveal the sequence of ketamine’s mechanisms and may be another explanation for ketamine’s lasting effects after it clears the brain, she says. “The lateral habenula may actually act more upstream of brain areas like the hippocampus.”
But there is no direct connection between the lateral habenula and the hippocampus, so this change in BDNF must be triggered by something downstream from the lateral habenula, such as its effects on serotonin production, says Joaquín Piriz, research fellow at the Achucarro Basque Center for Neuroscience, who was not involved in the new study. Future research should focus on better understanding the interaction between these two brain areas, he says.
Gould also adds that although mouse models are helpful, it’s important to recognize what translates to the human brain and what doesn’t: “A number of NMDA receptor antagonists, specifically lanisemine and memantine, have been tried repeatedly and assessed as antidepressants in people—and they aren’t. That’s the first thing I’d like to see is evidence that other NMDA receptor antagonists are antidepressants in humans, regardless of what they’re doing in mice,” he says. “Depression is really a human set of symptoms.”
Hu and her team next plan to research other molecular targets that help generate the burst-firing activity seen in the lateral habenula during depression. They have identified two other ion channels involved in burst firing, including a potassium channel on an astrocyte that is upregulated in depression.
Hu says she is also curious to see if other fast-acting antidepressants, such as psilocybin, act on the same brain regions as ketamine does.
“By seeing what ketamine targets, we may be able to understand what goes wrong in the first place,” she says.