As persons, we each develop and shape our individuality in our own ways, through the social and cultural resources accessible to us. No one tries to be an individual in the abstract; each person’s own sense of individuality, along with one’s sense of self and self-worth, is precious and irreplaceable. Bioethics need not deny these matters, but neuroethics has an extra responsibility toward these capacities. Neuroscience and neurotechnologies (neuroS/T), by centering on neurological functions, more easily affect and potentially impact the ways people experience being themselves. Not even the most reductive physicalism can deny that experience matters. (Science bereft of observational experiences would never confirm a single physical theory.) There is no need to embrace a dualism of body and mind, or to reduce the “self” or “individuality” to the brain, in order to grasp how the brain is not just another organ of the body. A brain working better is not just a better-working brain. An individual’s subjective world is also potentially at stake.
Neuroethical inquiry must ask—and try to answer—questions of how experiments and treatments affecting a person’s brain may translate into that subjective world, a person’s self-conception, and each individual’s own values. Neuroethics must be part of the watchful scrutiny over neuroS/T that checks for unwanted deviations from moral priorities such as self-integrity, mental health, and civil conduct. Whether newly invented or long adopted, implemented neuroS/T always involves more and more “research” subjects with each person who starts to utilize an innovation.
In 2002, the year that “neuroethics” was thrust into the academic spotlight, the journal Brain and Cognition devoted a special issue to this new discipline. The opening editorial by Judy Illes and Thomas Raffin surveyed the papers in this issue, noting how they cover ethical challenges in both basic and clinical research. Topics addressed included protecting human research subjects, patient privacy, communicating diagnostic findings, adequately interpreting findings from new brain imaging techniques, revising views of cognitive functioning as findings are interpreted, forming prognoses and predictions for patients, raising hopes about cognitive enhancements, and counseling patients about making meaningful and informed choices. These and related topics still form much of the core of neuroethical focus, and rightly so.
Primary duties toward human subjects and medical patients should be integral to experimental design. The hard ethical lessons from disreputable research learned anywhere should be respected everywhere. Upholding human rights for experimental subjects and recipients of clinical treatments cannot be abrogated, while nuanced ethical analyses can consider local values and norms to prescribe specific protections.
Like bioethics, neuroethics must support a robust and proactive stance toward gaining informed consent, minimizing risks of research, and safeguarding medical information. Diagnostics about a person’s neurological and cognitive functioning are among the most sensitive and private types of medical information, perhaps only comparable to genetic data. Research participants must receive due protection, as subjects of moral regard, by the medical and legal fields. That proactivity must extend to the “subjective” realm of the first-person standpoint, as a field of lived experience as well as a “data-point” of information, if there is to be a fully disciplinary neuroethics.
The moral problems and questions of ethics that flow from the stages of cutting-edge research and clinical application amply illustrate central neuroethical concerns for the meaning and morality of neurotechnologies as viewed by subjects themselves.
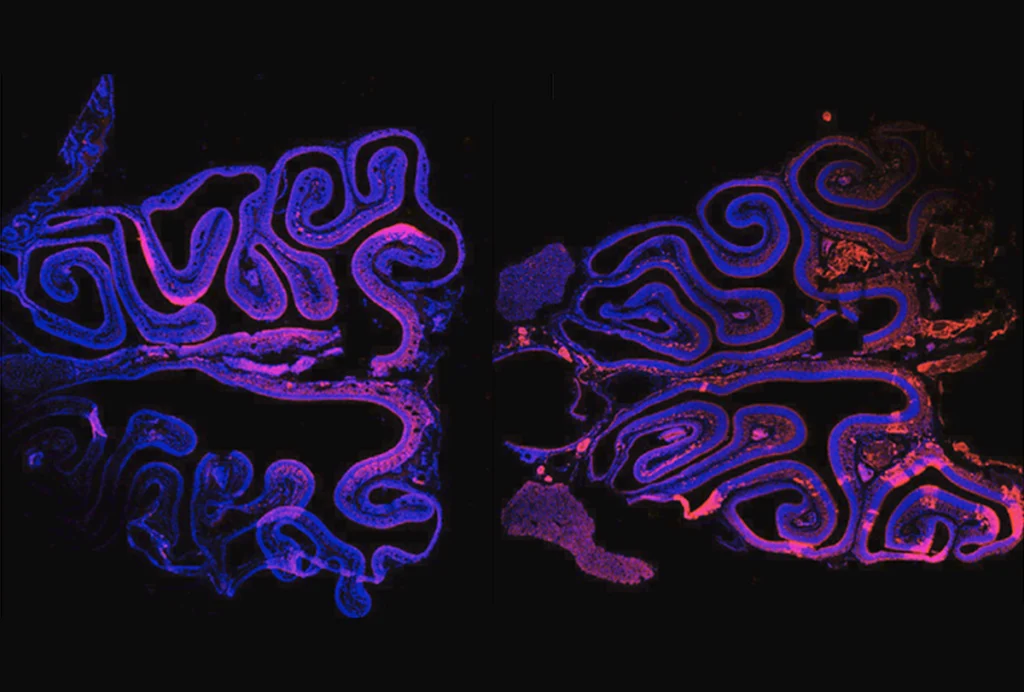
Neuroethics guides investigations into needed engagements between implementations of novel neurotechnologies and analyses of their ethical implications. These investigations can remedy the tendency to overlook the individuality and subjectivity of participants, where a focus on exacting precision and technical soundness predominates. For example, debates about neuroimaging to study “the brain” fixate on aggregated anonymized data, which sounds prudent enough until further questions are asked about the genuine interests and needs of participants. Underestimations of that neurotechnology’s tendency to erase heterogeneity, silence individual subjects, and ignore personal histories can easily ensue. The study of mental health through neuroimaging, for example, seeks to simultaneously connect one disorder with one neurological feature (such as the presence or absence of a certain systemic activity) for any human brain while also hoping to specifically predict that disorder in an individual brain with a single scan. Vince Calhoun, founding director of the Center for Translational Research in Neuroimaging and Data Science, points out how those two aims should not be conflated:
“The vast majority of brain imaging researchers focus on describing central tendencies and group results, rather than findings with individual subjects, and the case studies that are reported typically concentrate on explaining the data at hand rather than predicting unseen data from an individual (i.e., Can I use brain imaging to predict a future diagnosis, or to determine if that individual will respond well to a certain medication?). While this may seem like a small distinction, it is quite critical, as the results for these two approaches (studying averages versus studying individuals) often differ. A focus on individual level prediction and forecasting of future trajectories relevant to an individual person is arguably the most important goal if brain imaging is to translate into practical solutions to improve the quality of life and enhance technological development.”
Amassing as much data from as many subjects as quickly as possible, typically the goal of vast databases destined to serve public health issues, may overshadow due attention to private concerns.
Checking off a generic list of criteria for informed consent won’t necessarily suffice for vulnerable patients or populations. Downplaying risks, especially where no regard is shown for a participant’s medical history or current state of health, should not be tolerated in any country. The matter of incidental findings is also concerning; the variability found across research protocols remains a problem. Neuroimaging researchers themselves express concerns about adequate clarity and availability of ethical guidance about incidental findings. In 2010, a survey of guidance documentation from U.K. legislation, agencies, and medical councils and associations, along with European and international regulations, concluded by pointedly calling for better standardization across all types of medical imaging: “Discourse of national and international practice is required in the light of existing legal and ethical frameworks to develop robust and practical guidelines for both research centres and ethics committees considering proposals for imaging research.” Neuroethicists continue to notice a general lack of refinement and standardization for handling discoveries across all types of medical imaging.
Excerpted from “Bioethics and Brains: A Disciplined and Principled Neuroethics,” by John R. Shook and James Giordano. Reprinted with permission from the MIT Press. Copyright 2025.