When Andreas Horn began researching brain disorders treated by deep brain stimulation (DBS) about 10 years ago, he says he also started to wonder about the subthalamic nucleus: How could modulating such a small structure at the base of the brain help people with symptoms as different as tics, tremors and compulsions?
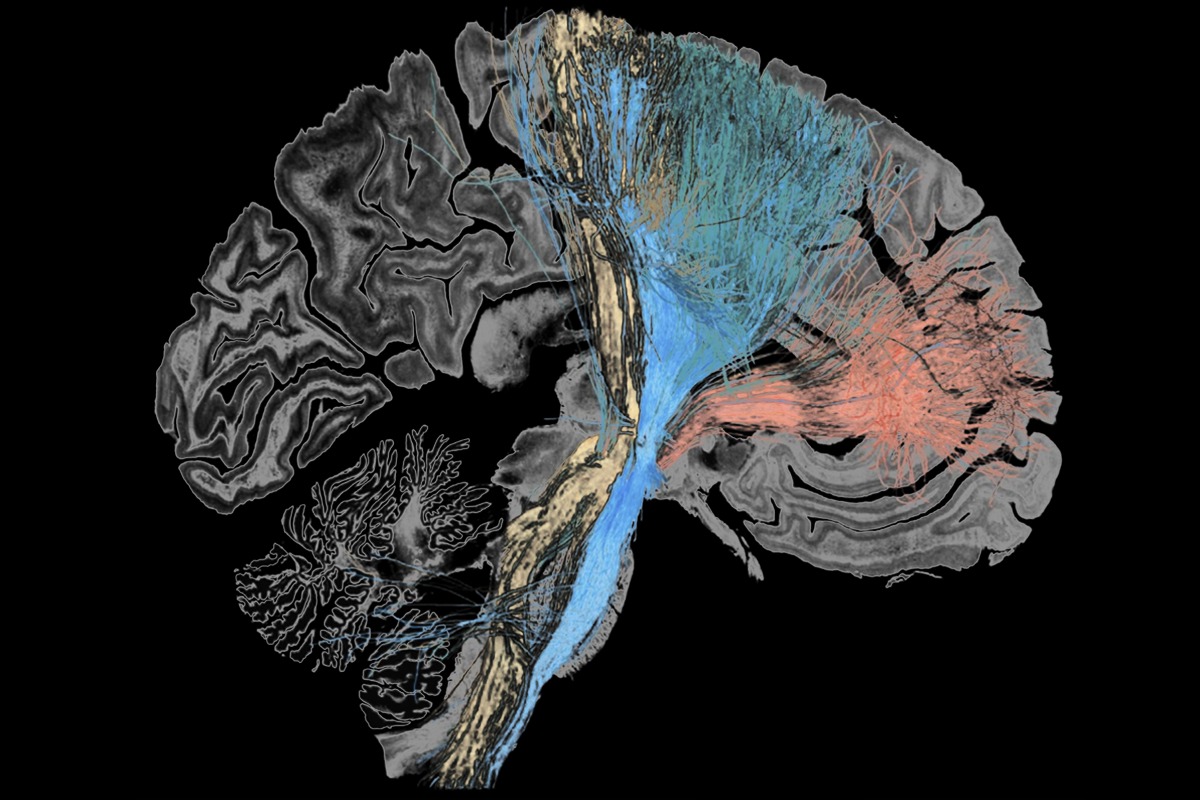
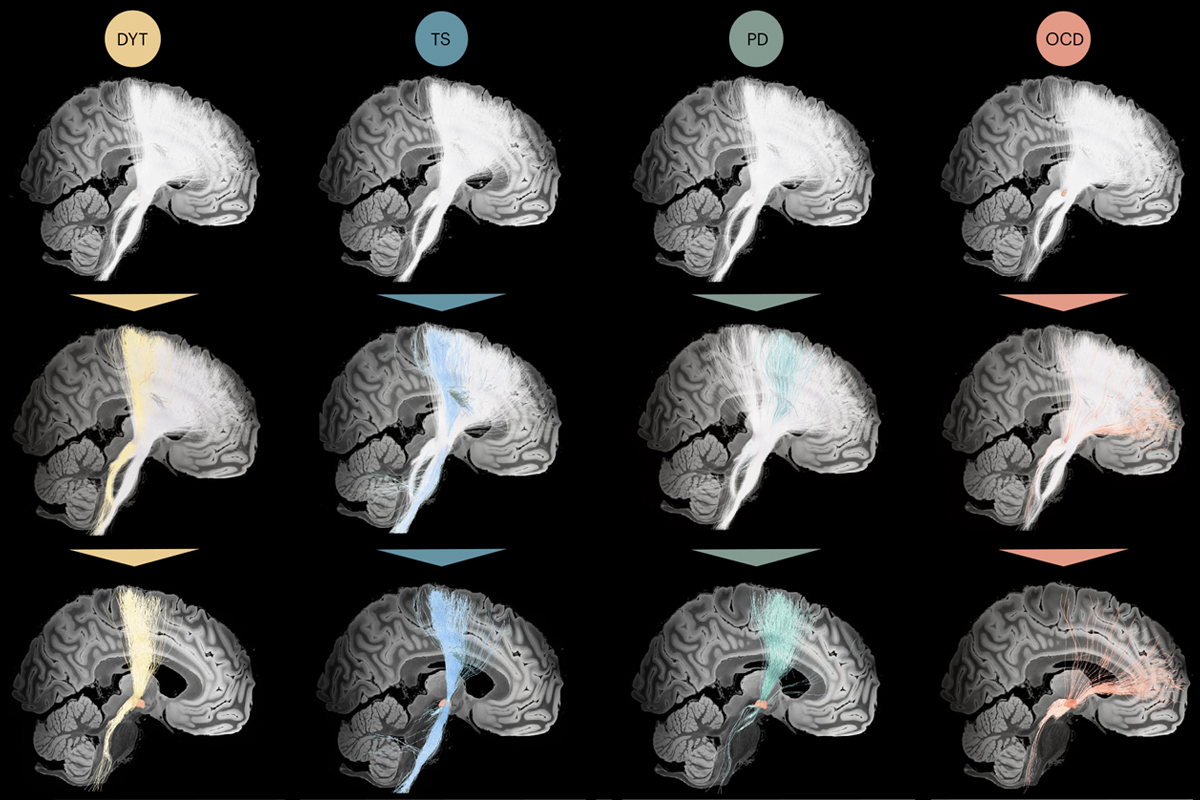
One reason is that targeting that area activates different circuits associated with different conditions, according to a new study led by Horn, associate professor in neurology at Harvard Medical School. He and his colleagues identified the circuits by locating DBS electrodes in brain scans from nearly 200 people with Tourette syndrome, obsessive-compulsive disorder (OCD), Parkinson’s disease or dystonia and plotting those locations onto a normative connectome of the human brain, created using diffusion tractography scans of hundreds of control brains.
The resulting “dysfunctome,” as Horn and his team dubbed it, shows the set of circuits likely to be disrupted in those disorders, Horn says, given that their activation via DBS is associated with symptom improvement.
That’s “not an unreasonable inference,” says Helen Mayberg, professor of neurology and neurosurgery at the Icahn School of Medicine at Mount Sinai, who was not involved in the study. “The subthalamic nucleus is a small area that’s a convergent zone for a lot of different pathways in the brain.”
H
orn’s work figures in an ongoing debate about how best to identify dysfunctional circuitry using diffusion tractography. The method, used to visualize fiber bundles in white matter, provides only an indirect assessment of axonal connections, “but it’s the best we have for noninvasive [measurements of] human brains,” says Sarah Heilbronner, associate professor of neurosurgery at Baylor College of Medicine, who was not involved in the study.A normative connectome built from tractography scans of control brains provides a low-noise comparison for scans from people with brain disorders, Heilbronner says, but other scientists, Mayberg included, say individualized tractography is needed to capture disease-related differences in anatomical connectivity.
“It’s [something] that we are fighting about relentlessly—there are different camps,” she adds.
Horn’s team purposely used a normative connectome in order to compare across diseases, says study investigator Ningfei Li, a research associate in the neurology department at Charité–Universitätsmedizin Berlin. They aggregated tractography data from 985 people without any brain disorders from the Human Connectome Project to form a connectome of 6 million fiber tracts.
“It’s still a bit controversial, I think, in the field,” Li says, but data from people with brain disorders are hard to come by and often of worse quality than the images included in the Human Connectome Project.
A software program developed by the team, called Lead-DBS, localized electrodes within the subthalamic nucleus on scans from 70 people with dystonia, 94 with Parkinson’s disease, 14 with Tourette syndrome and 19 with OCD treated at seven international DBS centers.