The first big surprise came sometime around 2014, Li-Huei Tsai says. A doctoral student in her lab at the Massachusetts Institute of Technology had come to her with an idea for an experiment: Hunter Iaccarino wanted to induce gamma rhythms in a mouse model of Alzheimer’s disease and measure the effects on amyloid beta levels in the brain.
Tsai’s lab had previously discovered how to generate gamma oscillations in the brain by way of optogenetic stimulation. But before Iaccarino proposed it, no one had attempted to associate those rhythms with any molecular, cellular or biochemical changes, says Tsai, director of MIT’s Picower Institute for Learning and Memory.
The experiment felt novel, Tsai recalls. And it took Iaccarino just one assay to show that inducing gamma oscillations optogenetically in the hippocampus at 40 hertz lowered amyloid beta levels in the mice—a finding so exhilarating that Iaccarino “ran down the hallway, ran into my office and showed me the plate readout,” Tsai says.
The next eye-opener came when Tsai’s group tested a new, noninvasive way to induce gamma waves—a light flickering at 40 hertz—in 5XFAD mice, a common model of Alzheimer’s disease. The light also lowered amyloid beta levels in the animals’ visual cortex before they developed any of the condition’s hallmark plaques. And even in mice with plaque deposits, the amyloid beta load was reduced.
When they published the results in Nature in 2016, they almost immediately garnered attention in the popular press and ignited discussions on Twitter (now X). “Holy s**t: evidence that 40 Hz visual flicker can treat Alzheimer’s,” wrote Mark Humphries, a systems neuroscientist at the University of Nottingham. The surprises kept coming: Tsai’s paper has since been cited more than 1,100 times, and at least two dozen entities have filed or been granted patents focused on treating the brain with some sort of stimulation around 40 hertz.
The frontrunner in that group is Cognito Therapeutics, co-founded by Tsai and MIT neurotechnology professor Ed Boyden, who co-led the 2016 publication with Tsai. The company has raised $128 million in venture capital funding, been awarded 11 U.S. patents protecting its technology and has advanced a therapeutic device—called Spectris—into a pivotal trial, with plans to report results to the U.S. Food and Drug Administration by the end of next year.
Nearly eight years after the initial finding, however, it still isn’t clear—to the MIT researchers or anyone else—just how 40 hertz stimulation might help reduce amyloid in the brain, and failed attempts to replicate the initial experiment have observers wondering if the idea of noninvasive stimulation for Alzheimer’s disease is just more false hope in a field long plagued by it.
There have been “numerous attempts to affect this biology in a lot of different ways,” says Bryce Mander, associate professor of psychiatry and human behavior at University of California, Irvine, and many of them looked good in mice but sputtered in humans. “We’ve cured mouse-heimer’s thousands of times,” he says. “We fail to cure Alzheimer’s disease.”
T
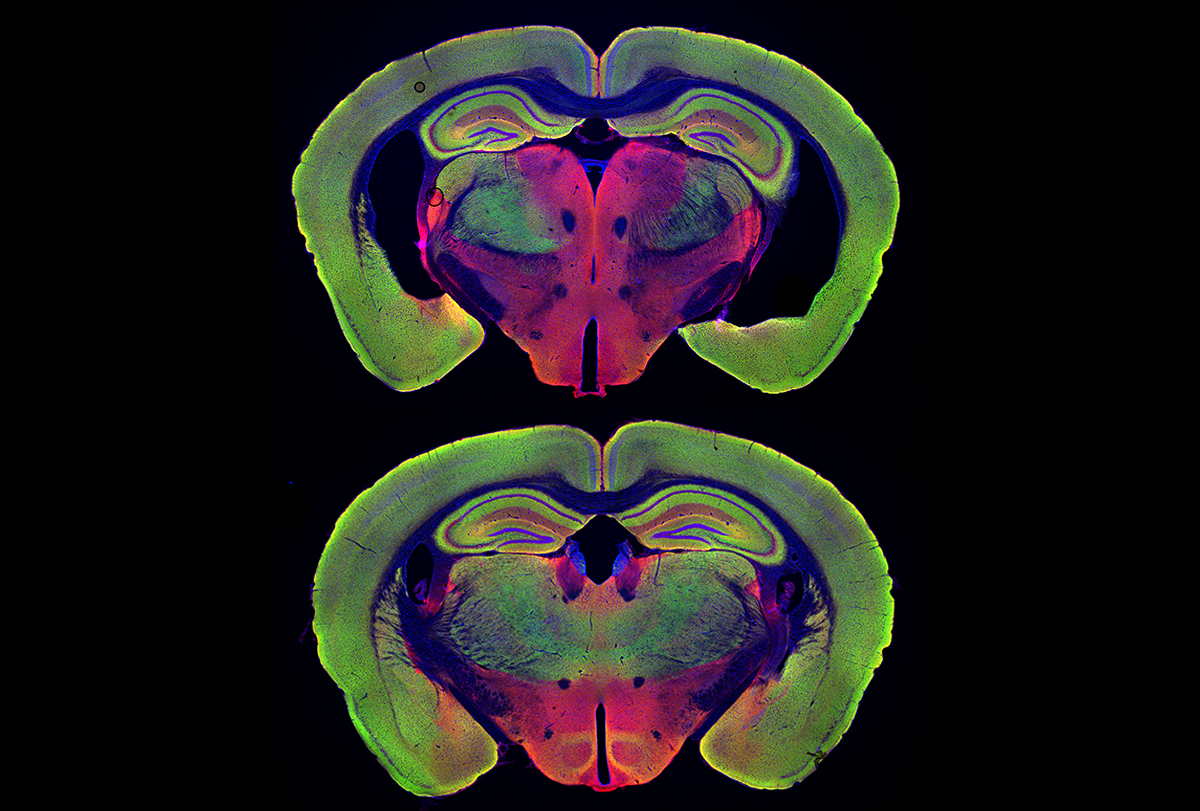
he work in Tsai’s lab was based on something researchers had realized years prior: People with Alzheimer’s have disturbances in gamma brain waves. Although these waves fall in the 25 to 100 hertz range, Tsai and her group found that stimulating the brain in mice at 40 hertz proved to be a kind of sweet spot: Optogenetic stimulation not only lowered levels of amyloid beta in the hippocampus, but also altered the shape of microglia in that region.The effect on microglia in particular seemed intriguing. Over recent decades, increasing evidence has suggested that microglia play a role in neurodegeneration, and it was shocking that noninvasive 40 hertz light might somehow thwart that process, Mander says. “That, to me, was amazing.”
Microglia also seemed to form clusters in the hippocampus, auditory cortex and prefrontal cortex when Tsai and her colleagues later induced gamma waves there in 5XFAD mice, using 40 hertz auditory tones in combination with visual stimulation. And the cells showed reduced inflammation after 40 hertz visual stimulation in two additional mouse models of neurodegeneration.
Despite these tantalizing clues, the link unifying gamma entrainment in the brain and a microglia response—never mind its apparently positive effects on plaques, memory, spatial learning and synapses—remained elusive. In the beginning, Tsai says, she and her team were convinced microglia were involved in clearing amyloid from the brain. But because a mouse model with depleted microglia still showed amyloid reduction after the 40 hertz exposure, now she thinks microglia “probably are not very important.”
Meanwhile, Cognito Therapeutics began developing a therapeutic device based on Tsai’s research in 2016. The Spectris headset combines glasses and over-ear headphones to produce flashes of light and pulses of sound, both at a frequency of 40 hertz. In 2018, the company launched a feasibility trial at Emory University and a phase I/II multicenter clinical trial dubbed OVERTURE. The company’s first patents came through in 2019.
When the OVERTURE study ended in 2020, 53 of the 76 participants enrolled had completed the trial, and it did not meet its primary endpoint: There was no statistical difference between the treatment arm and sham on the MADCOMS scale, a modified version of a clinical survey that assesses cognition and function in people with Alzheimer’s disease. Also, there was no change in amyloid in the brain, based on three PET scans over six months.