When I was 15 years old, I began using oral contraceptives to treat my acne. At 27, I decided to stop taking them, and my skin started breaking out again. I experienced light mood swings and irritability, common premenstrual symptoms I hadn’t had for the 12 years I was on oral contraceptives. Even more surprising was the fact that my menstrual cycle did not return for nearly five months.
These experiences highlighted for me the profound ways oral contraceptives can affect the body beyond their intended purposes. The medication had influenced not only my skin and cycle, but my mood and overall sense of well-being.
Oral contraceptives have been available since the 1960s and are widely used, but the study of their influence on the brain in particular—and, by extension, on cognition and mental health—is still a relatively new field of research. A quick search on PubMed reveals only 279 articles on oral contraceptives and mental health, as of 7 January, and just 124 that focus specifically on the brain and MRI. Most of the available studies are small, cross-sectional and narrow in scope, meaning they have a limited focus that makes them vulnerable to selection bias, confounding variables and reproducibility issues.
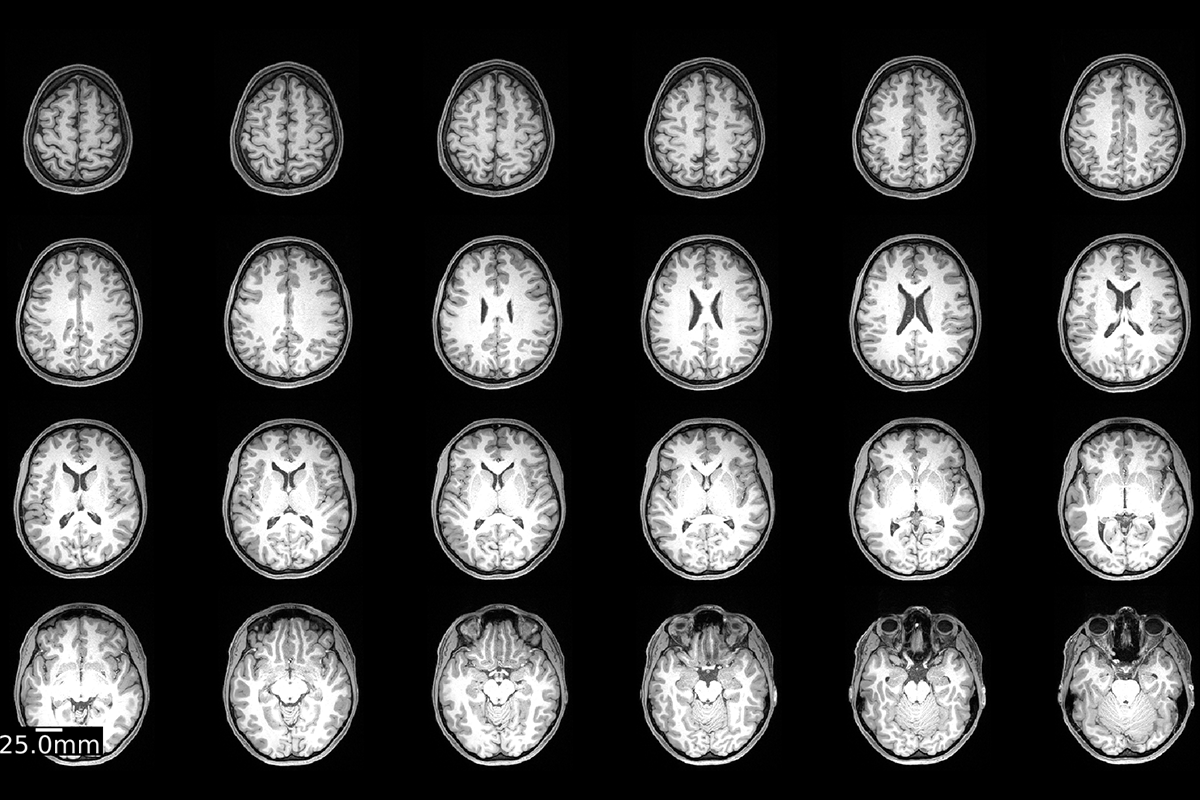
Motivated by my personal experiences and this knowledge gap, in 2022 I launched a one-person study using myself as the participant. Over the course of a year, I underwent 75 MRI scans and blood draws, both on and off oral contraceptives, to capture detailed information on hormonal shifts and their impact on the brain. By examining my brain in such depth across different hormonal states, I aimed to uncover within-person patterns of change that might offer new insights into how contraceptives influence physical and mental health. I chose myself as the research participant because I knew the process would be intense, and I knew I would be reliable.
I
was prepared for the work in other ways too. During my graduate work, I used brain imaging to study the biological underpinnings of schizophrenia. At the time, I was interested in oral contraceptives’ impact on the brain, but I hadn’t considered it a serious field of research or a viable path for a scientific career—probably because of deeply rooted bias in the field. After all, most biomedical research has historically focused on the male body, operating under the assumption that male anatomy and physiology represents the norm.This approach has left women’s health sidelined, subtly implying that these topics don’t matter enough for scientific investigation. But these issues are of vital importance. Globally, more than 300 million women rely on hormonal contraceptives, with 150 million choosing oral options. Though these medications are widely used for fertility control and safe family planning, they are also prescribed to manage a variety of health conditions, including endometriosis, polycystic ovary syndrome, irregular cycles, heavy menstrual bleeding, period pain, premenstrual symptoms, menstrual disorders, mood and other aspects of well-being. For many women, discontinuing oral contraceptives can have serious health repercussions. Because oral contraceptives provide such essential benefits, understanding their full range of effects—both positive and negative—is crucial.
The importance of this research also extends beyond individual health concerns. Access to contraceptives and reproductive care is essential, yet in some regions, this access is increasingly at risk. To make informed, personalized decisions about oral contraceptive use, women need to understand how these drugs affect the brain, how they might interact with a given person’s unique health history and which form of contraception might be the most suitable. In this way, scientific research plays a vital role in supporting women’s rights to manage their health according to their own needs and goals.
Pioneering work from several researchers inspired me to delve into this field. Emily Jacobs has examined the functional reorganization of the human brain during the menstrual cycle and other aspects of women’s brain health; Birgit Derntl is an expert in hormonal, affective and social neuroimaging; and Liisa Galea explores how sex, stress and hormones affect brain plasticity, specifically in preclinical models. Their contributions gave me the confidence to pursue this area of research and recognize its importance as a field of study.
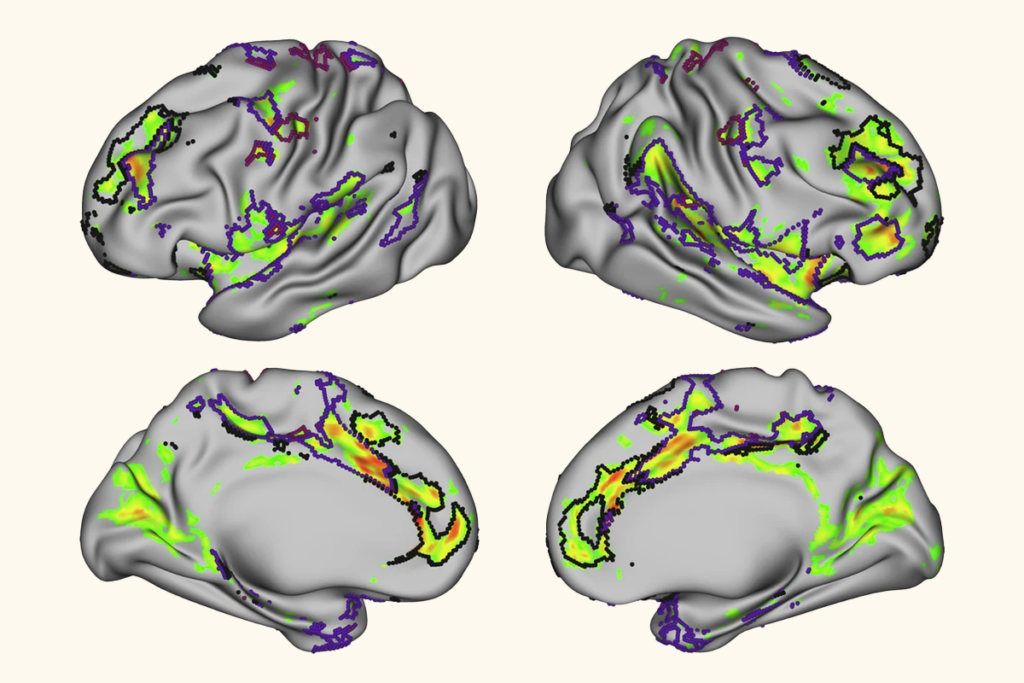
Their work, along with that of others, suggests that some differences in brain structure and function are tied to oral contraceptive use. But we still do not fully understand what these observed changes mean in terms of cognition, mental health or overall brain function.
To address this, it is time to move beyond small, cross-sectional datasets and focus on individual variability. Achieving a deeper understanding requires advanced study designs that can detect subtle but potentially significant changes in brain structure, function and connectivity over time. Unfortunately, progress in this area has been constrained, likely because of limited research funding, the historical underrepresentation of women in biomedical research, and other factors.
R
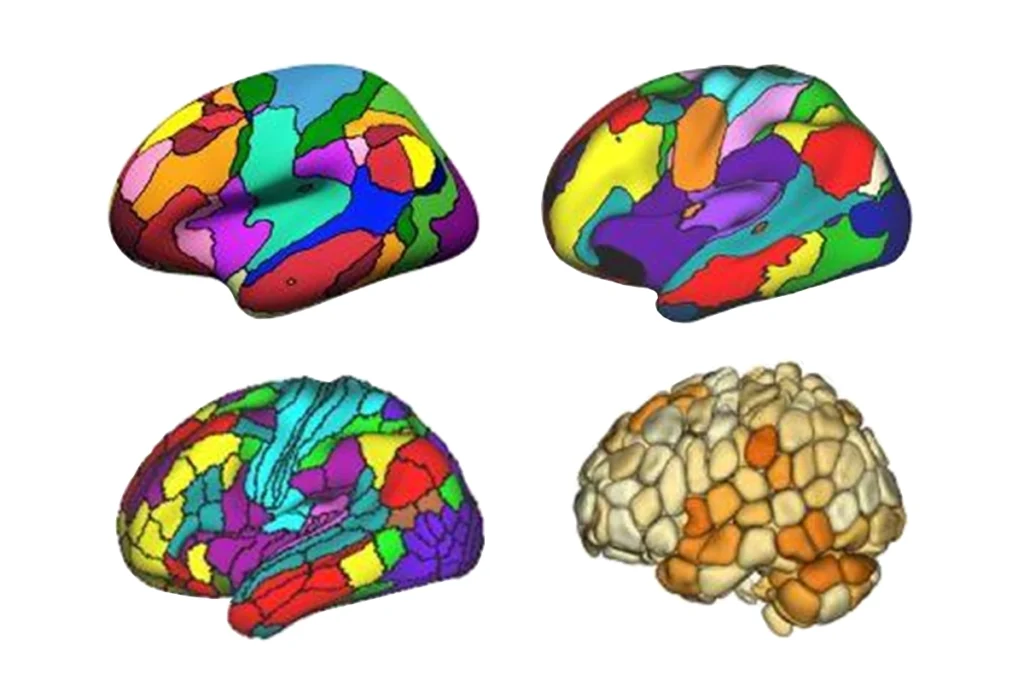
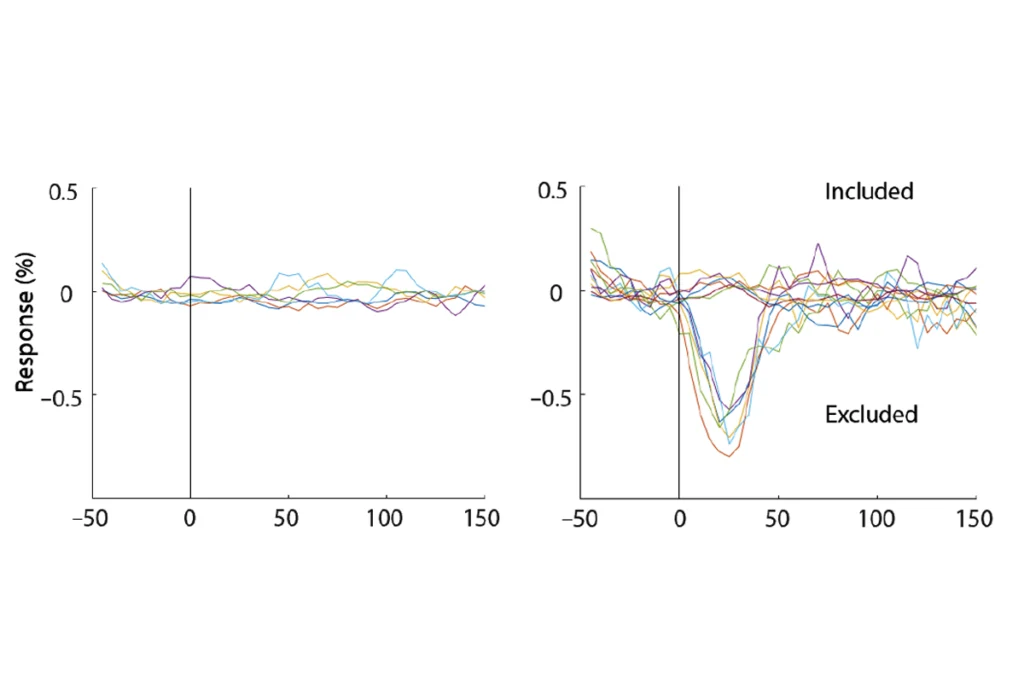
esearchers are employing two approaches to address the limitations of traditional small cross-sectional studies. The first involves big data from consortia-based projects, including the Women’s Brain Health Initiative and the ENIGMA-Neuroendocrinology working group, initiatives that pool new or existing data across multiple sites, increasing sample size and statistical power, and enabling more generalizable findings.My project falls into the second group: single-participant dense sampling, in which a participant is measured multiple times over a specific period. This approach is particularly revealing in studying hormonal cycles, because it enables us to observe shifts over time and minimizes external variables by using participants as their own controls. For instance, dense sampling can track hormonal fluctuations, brain activity and emotional changes in detail, revealing within-person patterns of variability that can provide a more personalized understanding of contraceptive effects.
Together, these approaches provide a comprehensive view; big data captures broad trends across groups, and dense sampling uncovers individual variability and nuanced patterns.
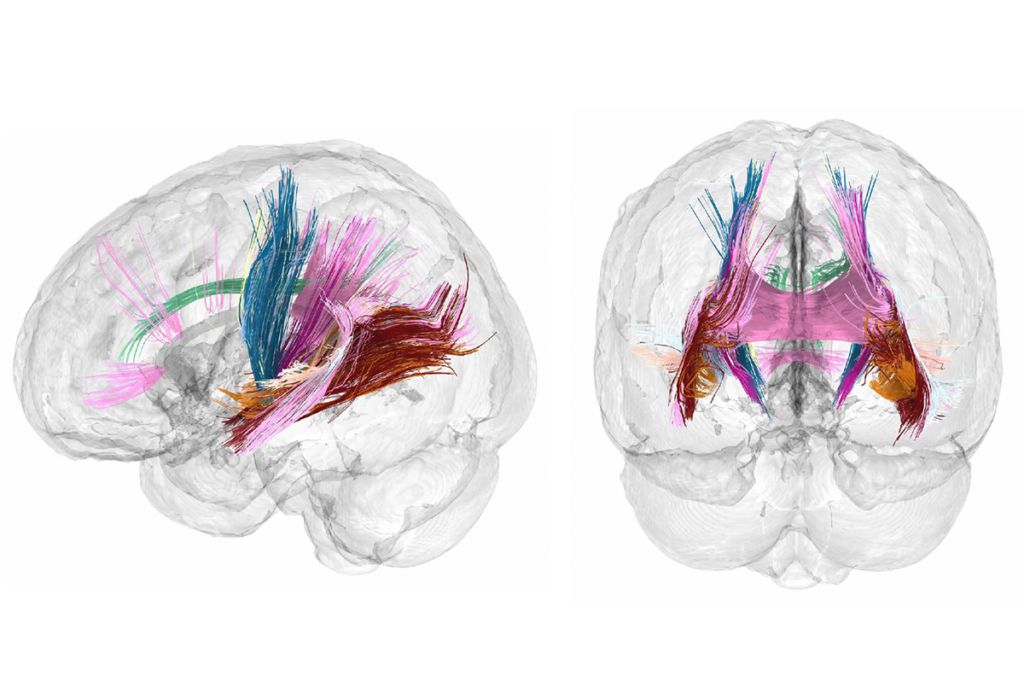
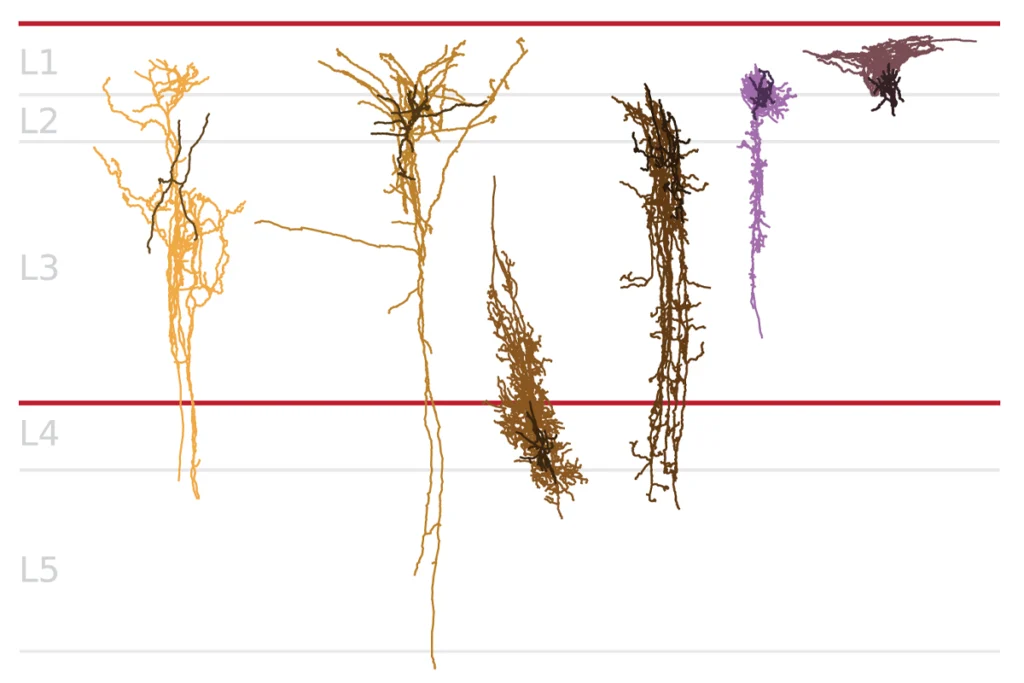
I’ve only just begun to analyze the data from my own brain, which includes structural, functional and diffusion MRI scans, along with blood samples to monitor hormonal dynamics—particularly levels of estrogen and progesterone. We also collected daily mood assessments, tracking positive and negative mood and anxiety. This dataset makes it possible to examine a variety of questions, such as how fluctuations in hormone level—during both the natural cycle and oral contraceptive use—might correlate with changes in brain connectivity and emotional variability over time.
Given the importance of transparency and collaboration in advancing women’s health research, I’m committed to making the data from my study publicly available once my analysis is complete. Other groups have done this as well, including Jacobs and her collaborators’ in-depth study of one person’s brain during and after pregnancy. (For more on that study, see “Repeat scans reveal brain changes that precede childbirth.”)
Open-science practices, including open access to data, enable other researchers to validate findings, address gaps and refine research methods. This is particularly important in women’s health, an area that has historically been underfunded and under-researched. Transparent data-sharing not only supports scientific accountability, it empowers women with evidence-based information so they can make informed decisions about their health.